It was the height of spring last year when mpox, formerly known as monkeypox, broke out among men who have sex with men — first in Europe and then all over the world. The outbreak coincided with a resurgence of planned trips and social gatherings after two years of COVID-related restrictions.
LGBTQ activists, public health advocates, and government leaders collaborated to establish a vaccination campaign coupled with targeted education to inform people about prevention and the risks of mpox. New York City opened sexual health clinics in some of the most impacted neighborhoods in multiple boroughs while local advocates prodded the federal government for more doses of the JYNNEOS vaccine.
The early days of the vaccination campaign were very messy. The rollout was hampered by limited supply of doses, equity issues, and technological glitches that prevented users from being able to sign up for the vaccine online. Eventually, the federal government cut through bureaucratic red tape and ramped up vaccine supply, while the city cleaned up its dysfunctional vaccine registration site and opened vaccination sites in the outer boroughs. At the same time, supply was stretched even further when federal officials improvised by directing health departments to inject the doses intradermally, which calls for using a fraction of a dose between layers of skin.
By the beginning of August, however, the virus had peaked in New York City — and after many months, it has now largely faded.
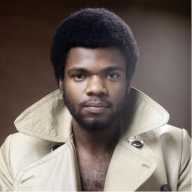
“We are certainly out of the worst of this, and as of January 9, we’re actually at zero cases per day compared to more than 70 per day during the peak of the outbreak,” New York City Health Commissioner Ashwin Vasan said during an interview with Gay City News on January 19. “Can we definitively say that it’s over? No, I don’t think we can say that. But the worst of this is over.”
Vasan credits the huge dip in cases to two key areas: advocacy and vaccine rollout. He commended the work of LGBTQ leaders and men who have sex with men who galvanized the community, drove behavior changes, and spread the word about resources, vaccines, and support.
“It’s important to remember that New York City was the first in country to launch extended post-exposure prophylaxis clinics in late June, and we did so knowing that vaccine supply was extremely constrained,” Vasan said. “But we did so knowing we couldn’t wait and we needed to drive the national strategy.”
Still, the vaccine rollout wasn’t as equitable as people hoped. There were complaints that too many of the doses were being allocated to white men, and Vasan pointed to “hidden data” indicating that lower rates of tests and vaccines among certain communities of color also meant that there were likely plenty of cases that went unreported.
The Health Department, Vasan said, responded with an equity strategy that focused on utilizing a network of community-based organizations and providers and using zip code restrictions, targeted referrals, and carve-outs for vaccination bookings in order to set aside doses for at-risk communities.
The process of actually bringing the vaccines to local neighborhoods, though, required effective community engagement, which Vasan said is where outbreaks “start and end.” The Health Department hosted town halls and numerous other events to engage with people and answer questions about mpox. The city then brought mobile vaccination vans directly to nightclubs and sex parties as part of an initiative that lasted through the fall.
“Once we realized we were past the peak, we knew we had to really get into the places with the highest risk, where if we didn’t address the need, we would see ongoing transmission,” Vasan said. “Our mobile vaccination sites were really innovative.”
Cumulative statistics on mpox cases in New York City by race/ethnicity show that Hispanic individuals make up 1,329 cases, followed by 1,050 cases among Black people, 859 cases among white folks, and 138 among Asian or Pacific Islander individuals. By gender, men account for 3,590 cases, while women make up 102 cases and transgender women represent 67 cases. There have been 53 cases among non-binary/gender-queer people, seven cases among trans men, and nine cases among those listed under “unknown” gender. By sexual orientation, 2,449 have been gay, 317 straight, and 1,062 unknown.
Cases, though, have dropped dramatically, to the point where there has only been one day with multiple cases through the first three weeks of the year. The numbers are largely in line with national trends, according to the Centers for Disease Control and Prevention (CDC). There were 40 cases nationwide on October 25, but that number dipped to 17 by November 25 and seven by December 25. There were just three cases registered on January 25.
The city is now contending with the challenge of keeping the virus at bay after spending months working to reduce cases.
It is not entirely clear, however, what the long-term plan is, at least for now. Vasan said there is no plan, at the moment, to administer booster shots, and he believes the vaccine is powerful enough to provide two years of protection — even from one dose — but conceded that more research is necessary.
When asked if the city is still employing the approach of using intradermal shots, Vasan paused before saying it “is still an active area of research and understanding.” The point of that method was to stretch supply, but demand has since dropped — and Vasan noted that intradermal mpox shots have not gained Food and Drug Administration (FDA) approval.
“That’s why the Health Department and city continues to offer subcutaneous vaccinations, and most providers are still doing subcutaneous,” he said. “Being in an emergency and an outbreak, the federal government made a choice to expand supply by using a different route of administration that they determined would offer a similar level of protection.”
The number one task at hand is to complete what everyone started when they went to get their first doses of the vaccine.
“We’ve done over 150,000 vaccines, but of those total vaccines, over 100,000 are [first doses], but only 50,000 are [second doses],” he said. “We need all of those folks who have only gotten one dose to come back and get their second dose. It’s recommended within a month, but it can be 90 days.”
He added, “We need people… maximally protected going into the new year and summer, where patterns will change and sexual behavior will change.”