Jacob Levine, who is currently on a PrEP regimen, at an August 13 meeting held at Ryan/ Chelsea-Clinton Community Health Center in Manhattan. | GAY CITY NEWS
While AIDS groups want a task force to write the plan that will reduce new HIV infections in New York from its current 3,400 a year to 730 annually by 2020, the Cuomo administration is moving ahead quickly with implementing major components of that effort.
“The message here today is no one else needs to become infected,” said Dan O’Connell, director of the AIDS Institute, which is part of the state health department, at an August 13 meeting held at the Ryan/ Chelsea-Clinton Community Health Center in Manhattan. “All of this is doable. Everything that we need is available today.”
While AIDS groups and the state expect to use a number of tools to reduce new HIV infections, the focus at the event was on pre-exposure prophylaxis (PrEP), or the use of a once-daily dose of an anti-HIV drug to prevent infection. PrEP is highly effective at preventing HIV infection when taken correctly, though failed adherence to the daily dosing schedule was a problem in PrEP studies.
Cuomo funds prevention effort at six clinics as formal plan for ending epidemic still taking shape
The Ryan Center is one of six health clinics in a state-backed PrEP pilot program that began in February and has recruited 80 people to date to use the HIV prevention tool. Also participating are the Asian & Pacific Islander Coalition on HIV/ AIDS (APICHA) and Harlem United in Manhattan, SUNY Downstate Medical Center in Brooklyn, Evergreen Health Services of WNY in Buffalo, and Trillium Health in Rochester. The clinics are meant to be the foundation for a statewide network to distribute a comprehensive HIV prevention effort that will include PrEP.
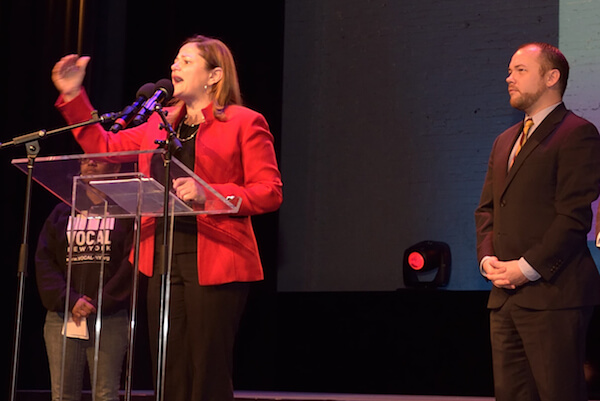
Dan O’Connell, director of the State AIDS Institute, at the August 13 meeting. | GAY CITY NEWS
AIDS groups began their push for a plan to end AIDS last year and won Governor Andrew Cuomo’s public endorsement in June after the state had already passed its budget for the current fiscal year, which began on April 1. Some health groups have been allowed to reprogram some state dollars to fund components of the plan, but any new dollars or major changes in what the state funds will be seen in the next budget.
“We’re going to be looking at this as a high priority in our next budget cycle,” O’Connell said.
Government funders have already been emphasizing HIV testing and getting people who test positive on to anti-HIV drugs so they are less infectious. They have also provided dollars for post-exposure prophylaxis (PEP), anti-HIV drugs to prevent infection in someone who experienced a recent exposure to the virus. PrEP and these other bio-medical interventions are the primary tools that will be used to reduce new HIV infections.
The August 13 event featured two panelists, Jacob Levine and Michelle Green, who are currently taking PrEP. They talked about PrEP as a practical tool that allowed them to take charge of their health and their sex lives.
“It’s for me to protect myself,” Green said. She noted feeling some embarrassment over taking the drug though her presence on the panel suggests she has overcome that.
PrEP was approved by the Food and Drug Administration in 2012. Some activists have suggested that the slow uptake of PrEP results from those using the HIV prevention tool being called sexually promiscuous.
“I struggled with that,” Green said, adding that she once hid her PrEP prescription so guests in her home could not see the pills. “I used to hide it, but then it wasn’t accessible to me.”
Michelle Green, who is also using PrEP. | GAY CITY NEWS
The state health department estimates that 3,149 Medicaid recipients in New York were taking PrEP from January 2014 through May 2014. That number does not include any New Yorkers who paid for PrEP with private insurance.
Using pharmacy data, Gilead Sciences, the company that manufactures and markets Truvada, the only drug approved for PrEP, had far lower numbers in two studies. The company estimated that 2,319 “unique individuals” across the entire nation started PrEP between January 1, 2012 and September 30, 2013. That increased from the estimated 1,774 “unique individuals” starting PrEP between January 2011 and March 2013.
Levine, a gay man, first became aware of PrEP about 18 months before he began taking the drug. He did not always use condoms during sex and was embarrassed by that.
“I have not had perfect condom use and that was something I was sort of ashamed of,” he said. Taking PrEP means he does not have to rely on others knowing their HIV status or HIV-positive sex partners taking anti-HIV drugs to reduce their viral load to be less infectious.
“I was scared by the prospect of relying on someone else for decisions that affect my health,” Levine said. “If you trust yourself to always use condoms, there’s no need for PrEP. That wasn’t my reality.”