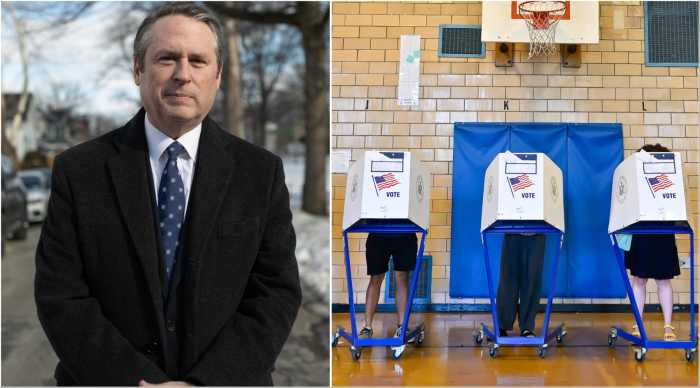
Health care costs continue to rise, forcing LGBTQ+ business owners and patients across New York to pay more for coverage and care. One of the reasons is that conglomerated health plans, pharmacies, and their third-party administrators profit from the 340B Drug Pricing Program, a federal initiative originally intended to help serve low-income patients by purchasing prescription drugs at a discount. But over time, it has transformed and now serves as a revenue stream for healthcare conglomerates — both vertically integrated health plans and pharmacies as well as large hospital systems. As a result, employers who offer health coverage pay higher premiums, while patients face increasing out-of-pocket costs. Before state lawmakers attempt to expand it, Congress should examine why a federal program meant to lower prices is making care more expensive.
A recent analysis found that large 340B hospitals charge commercial insurers an average of 7.5% more than their non-340B counterparts, adding up to $36 billion in excess spending each year nationwide. On average, outpatient procedures at large 340B hospitals cost nearly 20% more than at similar non-340B hospitals. That price difference falls especially hard on LGBTQ+ individuals, who often depend on outpatient services for essential care such as HIV treatment, mental health support, and gender-affirming services.
The problem is structural. Hospitals buy drugs at steep discounts but aren’t required to pass those savings along. Instead, they bill commercial insurers at full price and keep the difference. The health plans are also involved in the supply chain that benefits from the program. For patients managing chronic conditions and the businesses covering their care, the result is higher out-of-pocket costs and steeper premiums. In total, 340B growth added $23 billion in costs to employer health plans in 2023, with $4.5 billion of that paid directly by workers. New Yorkers are paying more so hospitals and giant corporations can turn the program into a revenue strategy instead of a safety net.
The profit motive under 340B is so strong that it’s reshaping how outpatient care is delivered. Hospitals can only apply discounts when drugs are administered through outpatient clinics they directly control, which has led many to acquire independent physician practices. Consolidation reduces competition, drives up prices, and limits patient choice. LGBTQ+ New Yorkers who rely on specialized, community-based care may find themselves redirected to systems that cost more and offer less personalized support.
The large institutions profiting most are spending little on the communities the program was meant to serve. One top 340B hospital in New York put just 1% of its budget toward charity care, which falls below the state and national averages. The savings stay with large hospital systems, at the expense of patients and employers.
340B is a federal policy, but its impact is felt locally. We know little details of how hospitals spend their 340B revenue or whether that translates to more accessible care for the most vulnerable among us. Assemblywoman Amanda Septimo (D-South Bronx) has introduced legislation that will create more transparency and ensure the program directly benefits vulnerable populations.
Access to affordable outpatient care is essential for many in the LGBTQ+ community, especially as healthcare costs continue to rise. The 340B program is no longer doing what it was meant to do. Expanding it without reform will only increase costs, reduce choice, and leave vulnerable patients and small businesses footing the bill.
Rev. Carmen Hernandez is a Bronx-based community advocate and activist, and founding president of the NYC LGBTQS Chamber of Commerce.