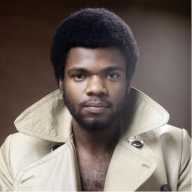
Jonathan Santos-Ramos, the director of operations at Callen-Lorde’s new clinic in the South Bronx, with staff member Luis Prieto. | CALLEN-LORDE COMMUNITY HEALTH CENTER
With Donald Trump’s announcement he intends to nominate Georgia Republican Congressmember Tom Price, one of the fiercest critics of the Affordable Care Act (ACA), as secretary of Health and Human Services, it’s clear the president-elect is determined to push his repeated campaign pledge to “repeal and replace Obamacare.”
Still, with nearly 20 million previously uninsured Americans now receiving coverage from their employers, through the network of health exchanges, or via expanded Medicaid eligibility, it’s impossible to predict precisely what the effort to dismantle the current president’s signature achievement will look like, particularly with both Trump and House Speaker Paul Ryan making favorable noise about retaining two of the law’s most popular features – the ban on insurers excluding pre-existing conditions from coverage and the ability of offspring up to age 26 to stay on their parents’ plans. How to preserve coverage for pre-existing conditions while eliminating the individual coverage mandate that most frequently draws the ire of GOP critics is something nobody has yet explained.
On top of the incoming administration’s hostility toward the ACA, there is also excited discussion among Republicans about reviving ideas, long kicking around, for turning Medicaid into a block-grant program in which states receive a fixed amount of money – anticipated to be significantly lower than current federal contributions – to do with as they see fit, and even for privatizing Medicare, the primary health insurance program for seniors.
At risk are individuals’ coverage but also federal support for community providers
All of which means that there is a lot of tough talk but few specifics coming from Trump, Price, and company – but also that the future course of American health care remains murky at best. That uncertainty extends beyond the issue of how individuals access care; it also raises questions about how advances in the nation’s overall public health infrastructure – gains unfortunately little appreciated in the debate over Obamacare – will fare going forward.
For LGBTQ Americans, a significant benefit under the ACA came in the form of the New Access Point program, which aims to improve public health in underserved and vulnerable communities by expanding access to culturally competent primary care. The “new access points” were 266 community health centers nationwide that were added to the stock of “federally qualified health centers,” non-profit institutions serving communities in need that enjoy substantial government support in doing their jobs. For the first time, five of those FQHCs had a specific focus on LGBTQ health needs, with two of them –– the Callen-Lorde Community Health Center and Apicha –– located in New York.
The advantages of the FQHC designation are significant. First, there is a $650,00 annual grant to offset the unreimbursed cost of care, which often represents a substantial burden on non-profits serving lower income communities. At the time of the New Access Point designations in the summer of 2015, Callen-Lorde, which serves everyone regardless of their ability to pay, reported its most recent annual unreimbursed cost of care at roughly $5 million a year in serving about 15,000 clients.
Likely more significant than the annual grants, however, is the ability of FQHCs to receive cost-based Medicaid reimbursement. Medicaid, a joint federal-state insurance program for low income Americans, typically reimburses based on a standard schedule of allowable payments that does not take a provider’s specific cost of providing care into account. This benefit, then, also contributes to lowering a health facility’s unreimbursed burden.
Including five LGBTQ-focused health centers among the New Access Point program represented unprecedented progress for the community. Earlier attempts by such non-profits to win FQHC designation failed, in part based on government officials’ concerns about their ability to serve non-gay patients. The 2015 designations, then, reflect a deeper understanding of unmet health needs within the queer community, something advocates will have to work hard to preserve in an administration whose appointees – including Price at HHS, Ben Carson at Housing and Urban Development, Betsy DeVos at the Department of Education, and even Trump’s choice of vice president, Mike Pence – have long and strong records hostile to the LGBTQ community.
Here in New York, the FQHC designation has meant more care in more places. On July 1 of this year, Callen-Lorde opened a new 3,500-square-foot clinic in the South Bronx on Third Avenue near 161st Street, its first footprint outside of Chelsea, and its patient rolls have increased from 13,000 in 2012 to about 17,000 by this year. Apicha, long based in Chinatown, is planning a new facility in Jackson Heights, Queens, while Callen-Lorde is investigating options for its presence in a third borough, in downtown Brooklyn.
Other statistics also suggest that the combination of Obamacare’s broader coverage and the FQHC designations have been beneficial for New York’s LGBTQ healthcare infrastructure. At Callen-Lorde, the portion of its patients who were uninsured fell from 37 percent in 2012 to 26 percent in 2015, while the number of those on Medicaid rose from 18 to 27 percent. Both trends suggest that increased coverage access and the Medicaid expansion under the ACA offered protection to a bigger chunk of the LGBTQ community; they also added to the greater financial security Callen-Lorde achieved by being an FQHC facility.
Last year, when Apicha won its designation, its CEO, Therese R. Rodriguez, said, “This is an important moment for the LGBT community. With these awards, the federal government is allowing us to reach out to the margins of the community — LGBT folks, immigrants, people of color, and people living with HIV/AIDS — to make sure they receive healthcare.”
Wendy Stark, executive director of Callen-Lorde, reflecting on what her agency has gained in recent years, put in even sharper relief what is at stake today. “Callen-Lorde serves as a critical safety net for thousands of people who are both uninsured and underinsured, as do community health centers across the country,” she told Gay City News in an email message this week. “Through the Affordable Care Act we’ve been able to help over 4,000 people become insured – which is of course beneficial to the health of those individuals but also to the overall healthcare system, because people who can access preventive care and treatment when they need it are more likely to stay healthier and be less reliant on emergency rooms and other forms of expensive care. Interrupting or reversing these advances would be truly devastating to the health of our communities and to the healthcare system at large.”
Whether those patients who now enjoy coverage either through exchanges or from Medicaid’s expansion will continue to do so in the Trump years is unclear. A wholly separate question is what the future holds for the nation’s FQHCs. It’s important to recognize that FQHCs were not a creation of Obamacare; they date back half a century to Lyndon Johnson’s War on Poverty, when they were created to address critical health disparities, largely at that time in inner city communities of color. The “New Access Points” program merely pushed the effort to offer care to more diverse underserved communities.
Significantly, since their introduction, FQHCs have expanded well beyond their urban roots, and now serve as critical primary care providers in many exurban and rural areas in every state. According to Kate Graetzer, advocacy and communications specialist at the Community Health Care Association of NYS (CHCANYS), the critical community-based care delivered by FQHCs across the nation has translated into “strong bipartisan support” for a program she said has grown “exponentially” and is highly regarded for its quality of services and ability to reduce costs. Nationwide, Graetzer explained, the program has been a “cornerstone of state efforts to streamline health care delivery.”
Tom Van Coverden, president of the National Association of Community Health Centers (NACHC), in a blog posting on that group’s website, echoed Graetzer, in part, by citing the “opportunities” afforded by the “incredible bipartisan support” FQHCs enjoy. He also, however, warned of “serious bumps [and] unexpected curves” as the result of November’s election. Beyond the immediate need for Congress to extend the basic financing authorization for health centers – no small matter, given the possibility of a 70 percent reduction in grant dollars if that is not accomplished – Van Coverden’s post and a memo NACHC sent to its member groups identified the repeal of Obamacare, with the potential for ending the employer mandate, exchange plan subsidies, and Medicaid expansion, along with a restructuring of Medicaid into some form of a block grant program as potential major “bumps” and “curves” facing FQHCs.
Neither the federal or state associations, however, would hazard guesses as to what is coming down the pike – in large part because neither the incoming president nor his Republicans in Congress have offered specific legislation or even detailed proposals, with a wide array of contradictory statements coming from Trump himself.
In his blog post, NACHC’s Van Coverden warned that FQHCs will have to “tell the Health Center story” and must do so with “data.” Graetzer, at CHCANYS, acknowledged that the higher rate at which patients have been insured since the enactment of the ACA has strengthened FQHCs’ financial position and ability to do their job, but she said it was not clear how repeal would affect those gains, especially given the strong constituency behind the FQHCs themselves.
Clearly, however, both associations are on what Graetzer termed “high alert” regarding the near future in Washington. As for health consumers, her CHCANYS colleague Steven Greenberg, who is the group’s external relations strategist, said, “They should watch what’s going on, they should learn what’s going on, and they should advocate not only for the continuation but also for the expansion of everyone’s right to health care.”