When MPV (or what’s sometimes called monkeypox) appeared in New York City in May, it came at the worst possible time. Our pandemic-fatigued city and exhausted public health workforce were already facing a COVID surge. We faced national supply challenges with MPV vaccines, tech glitches, and so many unknowns about the virus itself.
I don’t want to relive all of the challenges. They were real, difficult, and tested us all — especially the communities affected.
But that adversity is what makes where we are now so remarkable. New York City has administered more than 144,000 MPV vaccination doses. As our vaccination numbers rise, cases have declined — from a peak of more than 70 new daily cases reported to around five or less per day.
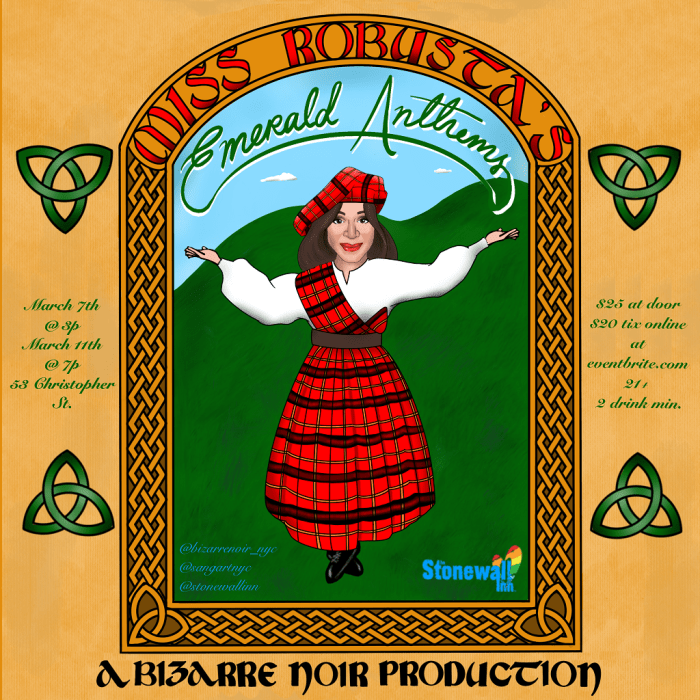
There are so many who’ve helped slow the spread. LGBTQ+ New Yorkers went to extraordinary lengths to protect themselves and their community. Community-based organizations engaged their networks to provide direct referrals for vaccinations and to share information. Bars, clubs, party promoters and so many others worked with us to get the word out, and to bring people in to care. Neighbors, caregivers, and family members protected those infected and isolating at home.
I’m immensely proud of our city’s response. We consistently broke new ground and pushed forward our local and national response — from being the first in the nation to expand vaccine eligibility and launching mass vaccination sites to developing innovative community partnerships and programs that have become a model for the nation. For example, New York City was first in the nation to launch so-called “extended PEP” vaccination clinics around Pride week in June. Despite the challenges in supply, we knew we had to act fast.
And those challenges along the way were not small. Disease response requires quick, urgent action. And with that, some degree of error is probable. Today’s mistakes, however, can be tomorrow’s successes. We just have to acknowledge them, study them, and see what corrections they demand.
Perhaps one of the most difficult observations in the response has been the racial inequities in vaccination. What makes these results so agonizing is that we saw them during COVID. We also see them in other public health indicators.
Health is littered with inequities, the byproducts of historical disinvestment and structural racism. Communities throughout our city are skeptical of government, and in the frenzied atmosphere of urgent disease response, a message of “trust us” doesn’t always work.
Building equity into disease response at the outset is a core tenet of our work at the NYC Department of Health and Mental Hygiene. For example, we partnered with trusted and credible messengers. People and organizations trusted by the LGBTQ+ and MSM community shared information regarding symptoms, how to reduce risk, and how to get vaccinated in multiple languages and media.
These leaders deserve praise for what they helped us achieve. Incredible work and collaboration took place during the MPV crisis. And when we engage communities together directly and consistently, we can overcome these inequities.
This is what we mean when we say we can never go back to the way things were done before COVID. New Yorkers are demanding the creation of a new kind of health equity infrastructure, grounded in partnership with community-based organizations and existing neighborhood networks. These networks must not only leverage community health workers. They must be based on shared planning, data sharing, financial architecture, and support, and program and performance evaluation. This will allow our community partners to evolve more deeply into the critical pillars of our public health delivery system in a more visible, coordinated, accountable, and effective way. Our community partners deserve a seat at our planning table, driving towards population health and equity goals together that are bigger than any of our organizations can achieve alone.
We’ve just begun this journey with the Public Health Corps — a partnership between our city’s Health Department and nearly 100 community-based organizations working in areas most impacted by COVID-19 — providing them with staff, support, and resources. We built this during an emergency, with the goal of getting people vaccinated, tested, treated, and protected with PPE as quickly as possible. We need a 2.0 version of this that builds on this emergent and temporary infrastructure applied to specific, pressing health challenges. This is how we can create a permanent health equity infrastructure and equity delivery system that addresses our long-term, chronic health inequities like diabetes, maternal mortality, and mental health while emphasizing prevention AND care — and one that is able to leap into response in the face of our next emergency.
As long as public health remains underfunded, we will not be able to build this sort of permanent public health and prevention infrastructure. These networks must be nourished and exercised. If they lay dormant between emergencies, they will wither, and the failures of past responses will repeat themselves.
The end result will prevent us from reaching our city’s and our nations’ health goals, whether during health emergencies or long-term health challenges. It will prevent us from addressing falling life expectancy and widening health inequities here in New York City and nationally.
We must leverage this moment and take lessons learned both — from COVID and MPV — to reinforce our call for transformative investment into public health. Our communities are depending on it.
Dr. Ashwin Vasan is the New York City health commissioner.