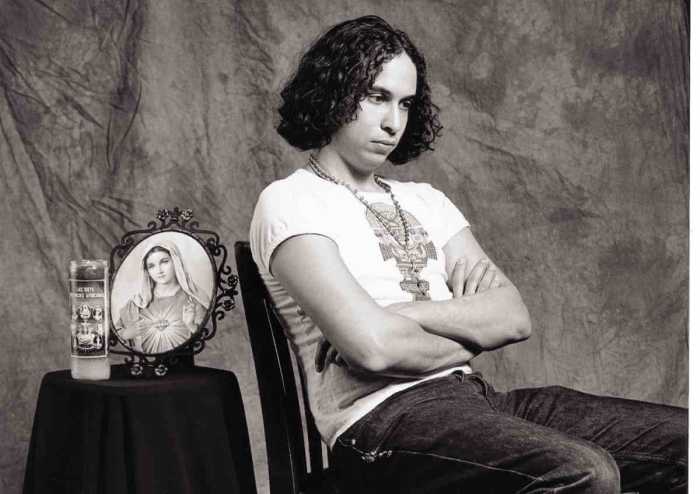
In the 20 months since Kelsey Louie took the reins at Gay Men’s Health Crisis in June 2014, he has consolidated operations from two floors to one in the West 33rd Street building where the AIDS agency is headquartered, cutting its annual rent by 25 percent. GMHC is looking for new space as its current lease ends in 2018.
Louie has “equipped the board and senior leadership teams with improved systems to ensure tighter management and efficiencies,” according to a memo he sent to the agency’s board that was shared with Gay City News in advance of an interview with Louie.
In addition to continuing to serve its HIV-positive clients, GMHC has expanded its HIV prevention efforts to promote pre-exposure prophylaxis (PrEP), anti-HIV drugs used by HIV-negative people preventively to keep them uninfected.
World’s oldest AIDS agency looks to healthcare delivery to the HIV-negative and positive
And by the end of 2016, it will open two clinics — one for mental health and another for substance use — because “untreated mental health and substance abuse are major drivers in the epidemic,” the memo said.
Further down the road, GMHC’s future lies in delivering healthcare services to HIV-positive and HIV-negative clients.
“This may be the continuation of reaching out to the non-HIV population,” Louie told Gay City News on February 19. “What are we doing to keep ourselves relevant and sustainable as AIDS goes away?”
When he took over GMHC, the agency had seen its revenues decline from 2007 through 2011. The move from Chelsea to West 33rd Street was controversial and expensive, as the agency was paying a high rent for space that it was not fully using.
In its 2014 fiscal year, 54 percent of GMHC’s dollars came from government contracts. That reliance on government cash can be dangerous because that money can be cut by politicians who are hostile to public health spending or government priorities can change. The ideal is a third from the government, a third from private donations, and a third from private insurers or Medicaid, the government insurance plan for the poor.
“We need to diversify our funding,” Louie said. “If we can really move to what I think is that sweet spot of a third, a third, a third, then any of these changes will impact a third of the funding versus 75 percent of the funding.”
GMHC was on the 63-member task force that drafted the Plan to End AIDS, an ambitious effort that aims to reduce new HIV infections in New York from the current roughly 3,000 a year to 750 annually by 2020. GMHC was founded in 1981 during the worst years of the AIDS epidemic, and the end of the epidemic means it must either close or change its mission. Delivering healthcare services to more than HIV-positive people is that new mission.
“Creating a new clinic with an HIV specialty doesn’t make sense if new infections are going down,” Louie said.
Currently, GMHC serves 9,000 clients annually and has a staff of 160. The agency has an onsite pharmacy, a hotline, hot meals, counseling and support services, financial management services, a mobile testing van that operates four days a week, and a clinic that does sexually transmitted disease and HIV testing. Those who test HIV-positive are walked to Mt. Sinai Hospital, GMHC’s partner, for treatment. Ninety percent of the clients of the two entities are virally suppressed, meaning they are healthy and cannot infect others.
“I would like to think that with our own healthcare instead of saying go four blocks, we can go down the hall or go down the stairs and we can capture some of that 10 percent that isn’t virally suppressed,” Louie said.
Getting into the healthcare business would likely be pricey and the market in New York City is consolidating, with providers growing larger. GMHC, with an annual budget of $27 million, is small, but it is a recognizable brand with access to a population — gay and bisexual men — that few other institutions have. The agency performs roughly 3,000 HIV tests every year, and about two percent of those tested are previously unidentified HIV-positive individuals. That means GMHC is testing the right people.
GMHC could grow bigger or it could merge with another provider, which might be controversial. As evidenced by the 30,000 people who joined GMHC’s annual fundraiser, AIDS Walk, last year, the agency enjoys a loyal following and those people may object to the brand being changed. Louie said there were currently “no serious conversations” about a merger.
A more immediate goal is getting the Plan to End AIDS funded. In the current fiscal, the Cuomo administration spent just $10 million on the plan. Charles King, the chief executive of Housing Works, an AIDS group, said last year that $104 million would be a “dream number.”
For the state fiscal year that begins on April 1, the Cuomo administration at first seemed to say that it would spend $200 million, but when Governor Andrew Cuomo released the proposed budget that commitment was for $40 million a year for the next five years. The plan’s “ambitious goal” can be met “with the proper funding,” Louie said.
“I think $104 million could be right,” he said. “I think $200 million sounds better. I think $40 million isn’t enough… More money needs to come upfront now.”