One of the first things I learned when I joined ACT UP in 1987 was that we could understand the science behind HIV without having PhDs or MDs. ACT UP remade the face of healthcare by proving that people dealing with a disease could understand the data behind it, and use it to make informed decisions. One of the ways I have survived with HIV for 37 years is by learning about this disease myself, rather than simply following the edicts of the experts.
So it’s disheartening that the same activists who inspired me to learn, and to teach others, about the medical aspects of HIV — which I’ve been doing since the late ‘80s — are now taking a very different approach. I’m now told we should not teach the data underlying the reports that people who have an undetectable HIV viral load have a much lower chance of transmitting the virus. Rather, we should simplify it to a catchphrase like “Undetectable=Unstransmittable,” because people can’t understand the nuances of the study behind it.
A closer look at “Undetectable=Untransmittable”
Really? Here are the facts: a number of studies have found that people who have an undetectable viral load, and who have been adherent to HIV treatment for at least six months, dramatically lower their chance of transmitting HIV. The most compelling data came from the PARTNER study, which followed 880 couples in which one partner had HIV and the other did not. The thing that made PARTNER stand out from other studies was that the only prevention tool used was having an undetectable viral load. No PEP or PrEP (drugs that can prevent HIV infection) or condoms were used.
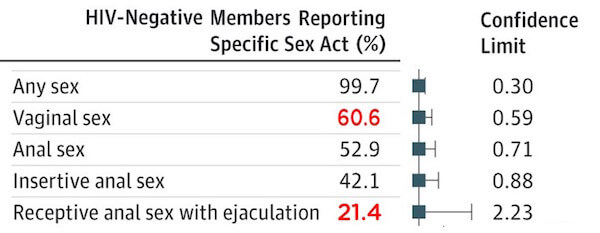
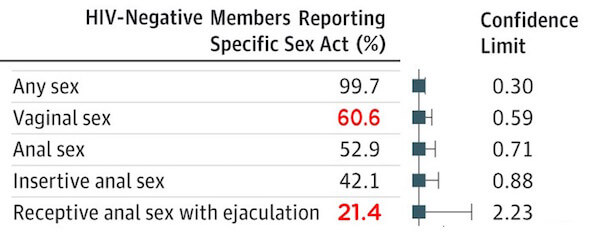
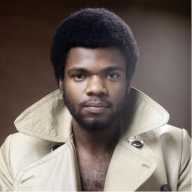
The data from the PARTNER study had a weaker confidence level regarding receptive anal sex than for vaginal intercourse. | COURTESY: PARTNER STUDY
When PARTNER found no transmissions in more than 58,000 sex acts, it was a game-changer. Soon, many experts and activists simply stated that U=U, with no caveats whatsoever. If your viral load had been undetectable for six months, you cannot transmit the virus. Period. And many people, particularly gay men, began using this information to make decisions about whether condoms were needed with a partner who is undetectable.
But when I actually read the PARTNER study, I found it wasn’t that simple. PARTNER studied both gay and straight couples, and looked at all kinds of sexual behavior. And the study clearly gathered enough data to show that the risk of transmission during vaginal intercourse was negligible. But when it came to receptive anal intercourse (bottoming) with ejaculation, the data was not as strong. While 61 percent of the HIV-negative people in PARTNER engaged in vaginal sex, only 21 percent bottomed during anal sex.
This led to a weaker “confidence level.” What does that mean? It’s a calculation based on how many people are studied and how long they are followed. For example, if a study followed only 50 couples for a year and found no infections, the confidence level would not be strong. But if a study followed 5,000 couples for 10 years, the confidence level would be very high.
So my first question was this: was the difference between anal and vaginal sex significant? Not being a statistician, I read the study carefully to see what its authors said. And they clearly stated that there was a real difference in the confidence levels for the two behaviors:
“Despite an observed transmission rate of zero for [anal sex with ejaculation]… an upper limit estimate of 20 percent risk over 10 years [cannot be excluded]… additional follow-up in MSM [men who have sex with men] is therefore needed… to provide equality of evidence between MSM and heterosexual couples, to inform both policy and also individual choice on condom use” [italics mine].
This does not mean that bottoming carries a 20 percent risk of transmission over 10 years. It means that the risk is somewhere between 0 percent and 20 percent — a broad range. So the same research team that did PARTNER is doing a follow-up study, PARTNER2, that is focused on anal sex (since it is the riskiest sexual behavior for HIV).
PARTNER2 is following about 950 couples (MSM and transgender women) for three years, to ensure that the data gathered for anal sex is equal to that gathered for vaginal sex. In order to do that, all researchers in the study have agreed to not release any preliminary data, but instead to wait until the study is complete, in 2019.
To many, “U=U” is a done deal, and no caveats need be presented. For example, when I brought up PARTNER2 at a community forum on “U=U”, the moderator tried to stop me by shouting, “People don’t need to hear that! You’re scaring them needlessly!”
Wow — when did information become scary? I’ve spoken to public health experts about this, and they agree that this information is important, but then do nothing to educate people about how to make decisions on condomless anal sex with someone who has an undetectable viral load.
For example, when my HIV-negative boyfriend saw the U=U campaign, he asked me if we could stop using condoms. I said we could, but first I told him about PARTNER2. I explained that this large follow-up to PARTNER was being done to ensure that the data on anal sex was equal to the data on vaginal sex. After he understood why PARTNER2 was being done, he said he’d like to wait until it reports its results before we take off the condom.
So my question is: did I have an ethical obligation to tell my boyfriend about PARTNER2? And if I did, do we all have an ethical obligation to tell anal bottoms about PARTNER2? I’m shocked that some of my activist friends say “no” — that it’s too complicated to explain and, besides, they’re sure PARTNER2 will find zero infections.
They also say, “There’s tons of data from other studies that prove U=U.” But when I actually looked at those studies, I found very little data on gay men who didn’t use condoms. For example, only 2 percent of the couples in HPTN 052 were MSM, and 96 percent of people in the study reported regular condom use. People also point to the “Opposites Attract” study (which also found zero infections) but that was a much smaller study, and the two cannot be combined due to their differences. PARTNER is the only large study I’ve seen that gathered significant data on anal bottoming without a condom, and even it didn’t gather enough to satisfy its authors — that’s why we need PARTNER2.
I’m also told that the positive aspects of U=U — the reduction in stigma, the reduced transmission, and the incentive to get tested and treated — outweigh the need to talk about PARTNER2. I agree that those are all important, but I don’t feel they negate the need for personal empowerment and choice.
It’s hard for me to write this and go up against so many people that I respect. But to me, the need for PARTNER2 is clear, as is my ethical duty to teach it. And the information is clear to people when I teach them. They thank me for telling them, and are angry that they hadn’t been told before.
I agree that PARTNER2 will most likely find no infections. But that’s not the point! (And if it does report no infections, don’t come to me saying, “I told you so.”) The point is: are we going to turn our backs on decades of patient empowerment and start making decisions for people based on our “expert” opinions? Do we now think that information should be withheld because we’ve decided people are too slow to understand it? That goes against everything I’ve worked for in 30 years of activism.
I can support someone ditching the condoms if they know about PARTNER2 and choose to rely on the experts, but almost no one I’ve talked to has ever heard of it! (And none of them has actually read the PARTNER study.)
So if people feel that U=U is a done deal, why don’t they recommend that PARTNER2 be stopped? It’s a very expensive, very long study, and if people think that questions about anal bottoming have already been answered, the study should be stopped. But if we don’t feel that way, shouldn’t people be informed as to why it is being done? Couldn’t we just say something like the following?:
“While experts are confident that U=U for all behaviors, people who bottom during anal sex should be aware that PARTNER2 — a larger, longer study focused on anal sex — is being done, since PARTNER did not gather as much information on anal sex as it did for vaginal sex. This study will report its results in 2019.”
My final caveat is that the data from PARTNER is being applied to situations very different from those studied. PARTNER followed long-term couples, in which the negative partner could be sure that their partner was undetectable, had been for six months, and was adherent. But if you meet someone on Grindr who says he’s undetectable, do you know he really is? And that he’s been undetectable for six months? And that he’s not missing doses? Extrapolating data from the couples in PARTNER to this scenario is questionable at best.
In the end, the issue is whether people who engage in the riskiest behavior for HIV have a right to know that a large study is being done on exactly that behavior. I think they do, and I’m disappointed that many of my peers feel they don’t.