A panel of health experts joined Amida Care and Gay City News on October 22 for an hour-plus-long webinar focused on the coronavirus pandemic and its impact on New York State’s plan to end the HIV/ AIDS epidemic, as well as other issues pertaining to the state of HIV prevention efforts.
The panel featured Doug Wirth, CEO of Amida Care; Johanne Morne, director of New York State Department of Health’s AIDS Institute; Dr. Anisha Gandhi, acting assistant commissioner and director of Racial Equity and Social Justice Initiatives for the New York City Health Department’s Bureau of HIV; Dr. David Collymore, chief medical officer and senior vice president of clinical affairs at Acacia Network; Dr. Asa Radix, senior director of research and education at the Callen-Lorde Community Health Center; and Ahmed Mohamed, a PrEP consumer and civic engagement and community organizer at the New Pride Agenda. Gay City News editor-in-chief Paul Schindler moderated the discussion.
The webinar came just days before the state health department’s second annual PrEP Aware Week, aimed at enhancing public understanding of the treatment’s HIV prevention benefits.
Panelists shed light on an array of relevant topics spanning from PrEP uptake to barriers to healthcare during the pandemic, cultural competency issues, and important statistical realities that have emerged throughout the course of a crisis that has forced the community to adapt to new circumstances.
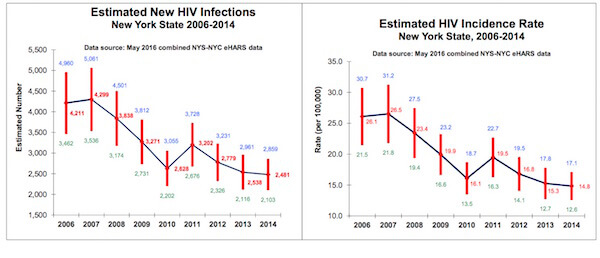
Morne — noting that full data on the state of the epidemic through 2019 will not be available until early December — laid out the epidemic’s contours as of the end of the prior year, pointing out that new diagnoses of HIV decreased and viral suppression among those living with HIV increased. She specifically spoke about a 38 percent decline in HIV incidence between 2014, when the state’s plan to end the epidemic was launched, and 2018, and to approximately 32,000 PrEP prescriptions in the latter year. On all of those indicators, Morne said, 2019 saw continued improvements.
The progress in 2018 and 2019, of course, came before the emergence of a coronavirus pandemic that forced those confronting the HIV epidemic to adjust on the fly.
Each of the panel participants talked about how their organizations made necessary adjustments to their work in response to COVID-19. Wirth elaborated on the different ways in which Amida Care, for example, shifted from in-person operations to remote work, identified pharmacies that could deliver medication to members, authorized medications to be filled for a longer period of time, and connected members to telehealth options.
Wirth’s team at Amida Care published a briefing paper last week outlining ways in which the coronavirus pandemic has impacted healthcare in New York, particularly surrounding HIV treatment and prevention, along with recommendations regarding how the state can stay on track to end the epidemic.
Collymore also said he and his colleagues at Acacia Network had to shift to telephonic and virtual options for patients, but the team noticed a strong need for in-person services, as well. The Acacia staff members were already back in the office within a matter of weeks of most of the city shuttering in the early spring.
“We saw that many of our clients and patients did not have access to technology or maybe did not understand the technology, so in-person services were absolutely essential,” Collymore said.
Radix pointed to some of the challenges that have emerged in HIV prevention efforts during the pandemic for those who are already on PrEP. Radix cited the difficulty in achieving regular lab testing and said some folks have had to turn to labs closer to their home that are not always LGBTQ-inclusive. One way Callen-Lorde has moved to alleviate that issue is to provide cultural competency training at labs.
“When people come to Callen-Lorde and get blood testing done, they’re in an affirming environment,” Radix said.
Radix also noted that Callen-Lorde has not seen as many new PrEP users during the pandemic as during a comparable recent period of time. One way conversations about PrEP are typically initiated is if a lab test reveals STIs, so a decline in such tests during the pandemic could be why the number of potential PrEP users did not grow at what otherwise would have been the expected pace.
Unsurprisingly, the pandemic has exacerbated issues that existed prior to COVID-19. For example, the lack of trans-specific advertising and trans-inclusive healthcare was already among the roadblocks hindering HIV prevention efforts focused on trans and non-binary individuals.
“Before you can initiate on PrEP, you need to have a discussion with a provider that involves a discussion about your personal risk, and many providers are just not equipped to discuss sexual health,” Radix noted. “And we need to do a much better job of that.”
In turn, the absence of trans-inclusive messaging has left some transgender and non-binary individuals wondering whether PrEP could negatively interact with hormone therapy, but Radix made it clear that is “not the case” and clarified that PrEP does not interfere with other gender-affirming interventions, including surgeries, either.
Panelists also pointed to a broader lack of LGBTQ-specific sexual health campaigns. Mohamed recalled his experience as an undergraduate at Duke University, where he said the institution places an emphasis on health and wellness but tends to steer safe sex outreach toward cisgender, heterosexual students. He said he first learned about PrEP through someone he was dating.
“Even when I would go get tested regularly, the local Duke doctor wasn’t the one who initiated conversations about being a potentially good candidate for PrEP,” Mohamed said, noting that he had to take the initiative to ask his doctor about it.
On that point, Gandhi acknowledged that she and her colleagues are aiming to deviate from the approach of identifying “candidates” for PrEP in favor of employing a more universal approach in which doctors inform patients more generally that PrEP is an option.
“We also want to make sure that all kinds of consumers that really may benefit from this are aware, and we’ve done that through social marketing, especially to make sure that we are dispelling misconceptions about who may benefit from PrEP,” Gandhi said. “We’ve talked a little bit about how we continue to see inequities and that PrEP is being utilized at greater rates among men who have sex with men who are white, and we are not seeing that same kind of progress with PrEP uptake among men who have sex with men who are Black or Latino, among transgender women, and cisgender women, even though they continue to make up a significant proportion of new diagnoses.”
Collymore jumped in at that point, acknowledging the gaps in medical providers’ expertise on that front. He conceded that Mohamed’s story is one that is “all too common,” and he compared the issue to the early days of HIV testing when he said many doctors were not testing for the virus. That was ameliorated when testing became more routine — and he suggested that doctors could be undergoing a similar warming-up period as they become more acclimated to PrEP.
As the coronavirus pandemic rages on — with record-setting numbers continuing to overwhelm communities across the country and around the world — panelists highlighted the importance of finding ways to continue making progress on the HIV epidemic in the face of profound challenges. Gandhi stressed that the future will depend on cross-collaboration between the government and other parties.
Looking ahead additionally requires experts to address racial disparities that have persisted even as New York has made strides in the 90-90-90 plan to get 90 percent of individuals living with HIV diagnosed, 90 percent of those diagnosed on treatment, and 90 percent of those on treatment virally suppressed. Forty-one percent of the 1,917 new HIV diagnoses in 2018 were among Black men, while 39 percent were among Latinx men.
Gandhi underscored the need for an approach that builds on the state’s Ending the AIDS Epidemic blueprint and combines “disruptively innovative” strategies predicated on being anti-stigma, intersectional, and community-driven, and are not “one size fits all” — even if the education effort is universal in its scope.
Collymore echoed Gandhi’s points and argued in favor of an individualized approach that, among other factors, takes mental health into consideration because it is connected to other aspects of healthcare — making the point that serious mental health challenges are often a bottleneck to addressing other health and social well-being issues.
“That 10 percent that we have not suppressed, we really need to look at each individual and see what needs to be done,” he said. “You cannot adequately treat someone’s physical health condition without addressing their mental health condition.”
Wirth added that pending legislative proposals could further move the needle in the right direction if lawmakers follow through. The effort to repeal a discriminatory loitering law known as a ban on walking while trans is an example of a piece of legislation that would help lower barriers to effective prevention outreach, while he also cited the continued lack of comprehensive sexual education in New York’s schools.
Revisiting what is covered under Medicaid should be another piece of the agenda moving forward, Wirth said, to better equip patients with the healthcare resources they need to take care of themselves.
“Why shouldn’t Medicaid cover a smartphone or the cost of a program so that members and patients could actually provide and get those healthcare services through the telehealth?” he asked.
On a broader level, Wirth called for a greater focus on bolstering economic opportunities for individuals living with HIV. He said providing those folks with a living wage could give them the breathing room so they could, in turn, offer peer help to others who just received a diagnosis.
Those who wish to utilize the city health department’s telehealth options can visit its Health Maps web page, which allows individuals to seek care tailored to their needs. Folks searching for providers offering PrEP services in their area can scroll the “services” sidebar on the left-hand side of the Health Map page and click on “LGBTQ Health Services.”
That tab will open up a range of options, including “Sexual Health Services.” Those services allow folks to find doctors that provide HIV testing, treatment, PrEP, PEP (post-exposure prophylaxis appropriate for the 72-period immedidately following a potential transmission event), or STI testing.
To watch the full webinar, click here or watch here:
To sign up for the Gay City News email newsletter, visit gaycitynews.com/newsletter.