Perry Brass wearing size large sweat pants to conceal the catheter a week after his radical prostatectomy, with his Riverdale neighbor Marnie Wood and his husband Hugh Young. | COURTESY: PERRY BRASS
BY PERRY BRASS | I woke up at 1:30 in the afternoon on Tuesday, June 14, in a recovery ward in Mt. Sinai Uptown. My robotic-assisted, laparoscopic radical prostatectomy, performed by Dr. Ash Tewari, had begun at 7:30 a.m., and six hours later, I felt fine, even if a little groggy, still enveloped in anesthesia and painkillers. I was examined several times by nurses who told me I was doing beautifully.
I didn’t want to look at my lower body; I’d have to face that later — when I was brought up to my room, hooked up to an IV feeding me antibiotics, painkillers, and glucose. I could have cold water, but no solid food until I passed gas. Carbon dioxide is pumped into your abdomen for the operation to extend it so that the “Da Vinci” robotic arm can get in there and do its work. The main way to release the gas is to… well, I had never wanted to fart so much in my life.
A month earlier, when I had first met with Dr. Tewari, the head of Mt. Sinai’s Urology Department, at Mt. Sinai Uptown on Fifth Avenue, he immediately drew me a diagram of how this prostate cancer intervention would go.
An invader in the pleasure dome: second in a three-part series
“I will make five incisions right here,” he said, pointing to my lower abdomen, “and then draw out your prostate from this one.” He pointed to an incision marked next to my navel. “The operation will take about 90 minutes. A day later, you should be able to walk a mile. The day after that, three miles.”
In that drawing, it all looked simple. After several months of numerous medical consults, I was so glad to finally settle the question of my course of treatment that I accepted everything he said calmly. We went into an examining room and he did a quick digital exam of my rectum:
“Yes, I can feel it,” he said. “We need to cut the cancer out of you.”
He then took me over to Denise Ramos, a young woman who is his scheduler and told her to book me for the operation. She opened a large scheduling book, and found the next available date: June 15. Exactly one month away. She then handed me a large folder filled with pre-op instructions and I put it in my backpack.
On the way back to Riverdale with Hugh, my husband, all I could think about was that this part was over. I didn’t have to go for another “second opinion” — I’d had plenty — and I felt altogether confident in Ash Tewari.
But it was still hard for me to accept that, at 68, I now had cancer. I glanced briefly at the inside of the folder, but avoided looking at it again for the next two weeks; I couldn’t make myself do it. I knew that every day brought me closer to the operation, and up ahead all I could see was a sense of panic settling in.
Two years earlier, I had had a transurethral resectioning of the prostate, or TURP, done to open my prostate enough so that I wouldn’t wake up to pee six times a night. The TURP performed at Mt. Sinai West (what used to be Roosevelt Hospital) was arduous. I was in severe pain for weeks afterwards, and had a raging infection that required more antibiotics. But in my mind I decided the TURP was a dress rehearsal for the prostatectomy. At least I had an idea of what this operation might be like, and how I would be afterward.
Following the TURP operation, it took five months for the benefits to kick in. I was finally getting up only once or twice a night to pee. Now, I was preparing to lose my prostate altogether — quite a zinger!
I had a difficult time telling people about the upcoming surgery. I dreaded that look of concern on their faces, and frankly it was hard to reveal that I’d fallen through the rabbit hole of cancer. My friend Mark Horn, who had been diagnosed with prostate cancer, or PC, eight years earlier, was scheduled to have his prostatectomy two weeks before me, and he reassured me, saying, “The decision who to tell is yours. It’s hard to talk about it, I know.”
About two weeks before the operation I went to a meeting of the Gay Men’s Prostate Cancer Support Group held the first Monday of the month at what was Beth Israel on Union Square (but is now called Mt. Sinai Beth Israel Union Square). I’d heard about the group, sponsored by MaleCare, a non-profit that works with prostate cancer survivors, through a flyer at Mt. Sinai’s radiology department.
One of the first to arrive in a large conference room, I met the moderator, Paul, and was impressed when 14 men showed up, ranging in age from their late 40s or early 50s to their 70s and 80s. The men were friendly, but not effusively so — prostate cancer doesn’t seem to inspire the same kind of bonding that, say, HIV often does. The men easily divided into two groups: those who had been treated, and were dealing with the problems and side effects of their treatment, and those who had not yet been, because they were either newly diagnosed or on what is known as Active Surveillance, a wait and see approach.
Hugh and others had warned me about support groups: they can be “iffy” because everyone’s story is different and it’s easy to pick up newfound fears there. It’s accepted wisdom that if you are not having post-treatment problems, you won’t go to a support group. As a result, there’s little chance of hearing from men who have gone through PC treatment and are now free of both cancer and major problems.
But that wasn’t really the experience I had. Some men went to the support group because only there could gay men with PC talk about it for 90 minutes without anyone either dozing off or telling them to get over it. And there was lots to talk about. Some men faced continued urinary incontinence after treatment and talked about where to get and how to wear “adult diapers” without feeling ridiculous as well as how to live with “accidents” that happen. Others discussed their trials in overcoming difficult sexual problems — including, sadly, potential boyfriends who run because getting an erection might require a post-treatment man to inject his urethra or penis with powerful, direct-delivery drugs. And still others gave vent to intense fear, depression, and, also, genuine anger — at urologists who still can’t deal with gay patients, at insensitive caregivers, or at hospital staff who piss them off.
I took notes and found myself choked up. Some of these men were so gallant, so brave, I thought, in dealing with all this. I learned that I would to have a Foley catheter inserted in my urethra during the operation and it would stay with me for nine days afterward to drain my urine. I hadn’t known this, but should have — it was in the folder I hadn’t yet read. I was also warned of the risk of dead scar tissue blocking urination, coagulating inside the urethra, and leading to an emergency room visit. Some men reported that they figured out they could take care of the dead tissue themselves by pulling it through their penis. I had to swallow hard hearing that, but was glad to know.
Paul, the facilitator, had to smile.
“This is something you don’t usually get at the regular support group,” he said, alluding to the value of a specifically gay support group. “They don’t talk about things so personally. There are a lot more barriers set up.”
A few days afterward, I finally went through the pre-op folder. It said I should be getting myself as strong as possible by exercising a lot, including doing Kegel exercises — a difficult series of squeezes to strengthen the pelvic floor muscles that undergird the pelvis. I was strong from constant daily exercise, but I had not been doing Kegels — and despite finding online instruction in doing so, I didn’t make much progress. Interestingly, women and an increasing number of gay men use these exercises to improve the quality of their orgasms.
I wasn’t happy that my operation was set for the very middle of Pride Month, and would mean my missing parties and maybe even the parade itself. I’d read that my exercise for six weeks after the operation would be limited to walking and lifting no more than eight pounds. Having exercised virtually every day of my life — doing Pilates, full body exercises, and interval aerobics — I was convinced my body would fall apart completely my first week without that.
Visiting Mark Horn at Mt. Sinai Uptown the day after his operation, I found he looked good considering what he had been through. He was being released — no one stays in hospitals very long these days — and I helped him out of his hospital gown and into his clothes. I got to see his incisions and also his catheter. That was difficult, but I had to face it.
My week leading up to the scheduled operation on Wednesday, June 15, was packed with tying up loose ends, so I was caught up short when I got a call on Monday that it was being moved up a day to Tuesday. I was expected at Mt. Sinai at 5:30 a.m. the next morning. The pre-op instructions asked for a light diet leading up to the operation and a 24-hour fast immediately beforehand, but Denise Ramos assured me, “You can have a light dinner before, just nothing after midnight.”
Suddenly I snapped to attention. I could do this — and having one day less of anticipation meant less time to get nervous. I went to bed early, woke up at 4 a.m., got some exercise, did a pre-op Fleet enema, and dressed. Then I started worrying about the change of clothes needed for the day I’d be released, and I began throwing things in my backpack like crazy. I realized this was the only way I could face this, as if I were going away on a trip and needed to pack for it thoroughly.
Hugh drove me downtown from Riverdale and when we arrived at the surgery holding area, I figured I’d be sitting there for a while. Instead, everything started instantly: intake, resolving insurance questions with billing, seeing an intake nurse who was very sweet and comforting, then out of my clothes and into a gown, saying goodbye to Hugh. It all happened so fast, I had that feeling someone else was doing it.
On the surgery floor, I saw Dr. Tewari for a moment; he too was positive and cordial. Then I met my anesthesiologist, a very matter-of-fact young man who started an IV line in my left hand. The line was taped to me, I peed again, and was then walked into the operating room. To me, operating rooms have a very theatrical quality — you feel like the audience for a moment, and everyone is performing for you. Surgeons love music; they were playing Frank Sinatra: “Fly me to the Moon, let me play among the stars…”
I felt good. Tewari’s assistants smiled, I was positioned on the table, and told in a second I’d fall asleep. And of course I did.
When I next saw Hugh, in my room, he asked how I was doing. I felt great — painkillers again — and also twitchily energetic, like my body wanted to bounce out of bed, even though I was also exhausted. Hugh told me Tewari had said the operation was a real success. “There was no cancer in your pelvic lymph glands or the margins,” meaning the areas between organs, Hugh repeated. And soon enough, Tewari himself turned up, shook my hand, and confirmed Hugh’s report.
It’s important to start walking after surgery to prevent blood clots, and, within several hours and with a nurse helping me, I was walking around the ward, still attached to my IV pole and with a catheter draining urine out of me.
By 7 p.m., I started a round of groggy phone calls with my friend Ricardo Limon as well as my sister Nancy from San Antonio. I was already impatient due to my fatigue and hunger, with Jell-O and clear broth my only food options. Finally, around 8, it happened — the gas passed! I was so relieved. At 11, with a nurse’s assist, I went for another walk, feeling more secure on my feet now. It was good to be occupied because the idea of sleeping in the hospital suddenly terrified me.
Cancer once again sent me into a panic. The hospital room’s clinical coldness. Being alone and knowing it. I called the nurses’ station and asked if they could give me something for anxiety. A pharmacist came in with one Zoloft pill. I took it, and a short time later fell asleep.
I left the hospital the next day, with full instructions on how to deal with the incisions on my stomach as well as with the catheter, and a goody bag of catheter supplies (plastic bags for urine collection, bandages, gauze, and more) and six prescriptions for drugs I’d have to take for the next two weeks, including antibiotics and two painkiller alternatives: 800 ml ibuprofen and Percocet, the latter of which I avoided as much as possible.
I was so happy to be back home, doing daily walks to build up my strength and eating real food again. I learned how to empty and change the catheter bags myself — a daily one attached to my leg and a night bag stored in a plastic pan next to my bed. The catheter didn’t especially bother me; I was energetic enough and free from pain due to the ibuprofen that most of the time I was able to enjoy myself walking outside, soaking up June’s weather, or reading, free of thinking about cancer and what I had gone through.
What I did not yet realize was that I was only at the beginning of my recovery.
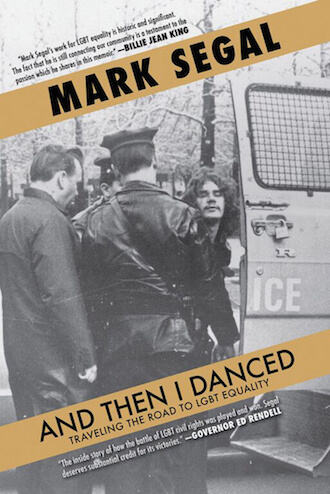
Next installment: “An Invader in the Pleasure Dome — The Recovery and Facing Life After Prostate Cancer.” (Check out installment one here.) A gender rights pioneer and award-winning writer, Perry Brass has published 19 books, including poetry, novels, short fiction, science fiction, and bestselling advice books (“How to Survive Your Own Gay Life,” “The Manly Art of Seduction,” “The Manly Pursuit of Desire and Love”). A member of New York’s radical Gay Liberation Front, in 1972, he co-founded, with two friends, the Gay Men’s Health Project Clinic, the first clinic on the East Coast specifically serving gay men that is still operating as the Callen-Lorde Community Health Center. Brass’ work, based in a core involvement with human values and equality, encompasses sexual freedom, personal authenticity, LGBT health, and a visionary attitude toward all human sexuality.