BY DUNCAN OSBORNE | As government funders increasingly pay for biomedical interventions that prevent HIV infections, such as pre-exposure prophylaxis (PrEP), and provide less support for behavioral interventions that increase condom use and alter sexual behavior, the funding landscape for AIDS groups may shift and they will have to change how they interact with their HIV-negative clients.
“That’s a major challenge that the community doesn’t know that PrEP is an option for them,” said Kimberleigh J. Smith, vice president for policy, advocacy, and communications at Harlem United. “It’s a whole different conversation that has to happen with folks… It’s going to come with a different level of engagement.”
Harlem United, which hired its first fulltime PrEP navigator in January, performed just over 4,500 HIV tests in 2014 and roughly 2,600 were on young men who have sex with men, a population that has a high rate of new HIV diagnoses. Smith said a “fair amount” of those were repeat testers, likely people who are having frequent or intermittent unsafe sex and keep getting tested to monitor their HIV status. Previously, repeat testers could be offered counseling; now they may be candidates for PrEP, a regimen of anti-HIV drugs HIV-negative people take to keep them uninfected.
$185 million in new CDC grants continue trend away from behavioral to biomedical interventions
PrEP, post-exposure prophylaxis (PEP), which prevents infection in HIV-negative people with a recent exposure to the virus by giving them anti-HIV drugs, and treatment as prevention (TasP), which is the use of anti-HIV drugs by HIV-positive people to reduce the amount of virus in their bodies to the point they are non-infectious, are highly effective when taken correctly.
The challenge with these biomedical interventions is letting people know they exist. Approved in 2012, PrEP uptake has been slow, though it is increasing. PEP has been used for more than 20 years mostly by medical professionals with a recent HIV exposure, such as a needle stick, and it remains relatively unknown and underutilized. TasP has been partially successful in New York City. The interventions require medical follow-up and support to adhere to the drugs.
Government funders, who were already moving away from paying for behavioral interventions and paying instead for high-volume HIV testing and getting those who test positive into treatment, are moving even more of their money into biomedical interventions.
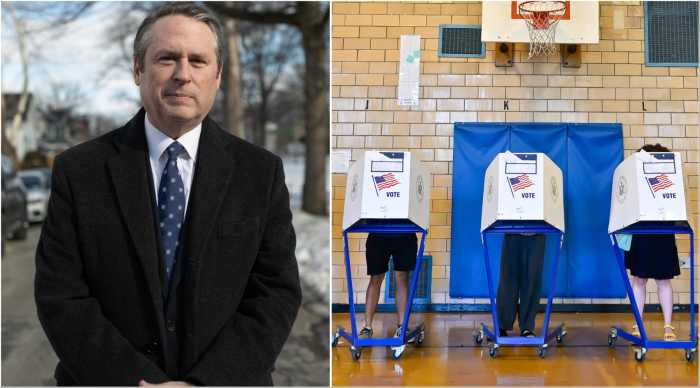
On March 31, the federal Centers for Disease Control and Prevention (CDC) announced $185 million in available grants for state and local health departments to fund PrEP and TasP demonstration projects among men who have sex with men and transgender people. Roughly $65 million of that is for projects targeting gay and bisexual men of color.
When Governor Andrew Cuomo endorsed a plan last year to reduce new HIV infections in New York from the current 3,000 annually to 750 a year by 2020, his first action was to negotiate lower prices for the anti-HIV drugs the state buys. In the state budget for the fiscal year that began on April 1, Cuomo included $5 million in new funding to pay for PrEP-related costs for an estimated 600 people, though that program may turn out to cover more people.
The shift in funding favors larger organizations that do a lot of HIV testing and have onsite medical clinics that can perform the follow-up testing needed for PrEP and TasP. People who are finishing a 28-day PEP regimen could be PrEP candidates and agencies need staff who can talk to that population about PrEP.
“We’re scaling it up,” said Robert Cordero, president and chief program officer at BOOM!Health in the Bronx. “We’re going all in on PrEP.”
BOOM!Health was formed by a merger of CitiWide Harm Reduction and Bronx AIDS Services. The agency has an onsite clinic operated by Brightpoint Health, a pharmacy, and it has partnered with the Callen-Lorde Community Health Center, which is headquartered in Chelsea, in a soon-to-be opened Bronx wellness center. Callen-Lorde is a leader among institutions in writing PrEP prescriptions.
Last year, BOOM!Health performed 5,000 HIV tests. While the agency currently has “less than a handful” of clients on PrEP, Cordero said, they plan on offering PrEP to drug injectors, couples in which one partner is HIV-positive and the other is not, and other HIV-negative people.
“I’m way more competitive than my peer agencies because we have healthcare onsite,” Cordero said.
AIDS groups were already merging, getting bigger, and offering medical services in a single location. The push toward biomedical interventions may complete that trend. The future for smaller AIDS agencies is uncertain, though their links to specific communities will remain valuable.
“We have been able to build strong access to social networks,” said Guillermo Chacón, president of the Latino Commission on AIDS. “Many organizations like ours are essential to making that bridge.”
The commission is among those AIDS groups, including Gay Men’s Health Crisis, that have affiliations with outside medical providers, but do not provide the kind of onsite medical services needed to support PrEP, PEP, and TasP. GMHC did not respond to a request for comment.