Health dept. numbers temper view on risk for young men of color
New data from the city health department may challenge widely held beliefs that new HIV infections are happening mostly among young men who have sex with men (MSM), most of them African Americans, and that HIV infections are increasing among gay and bisexual men.
In 2002, 72 percent of new HIV diagnoses among gay and bisexual men in New York City were among men over 30 and 41 percent of those men were white. Thirty-three percent of the men over 30 newly diagnosed with HIV were African American and 24 percent were Latino. The remaining two percent were men of other or unknown race or ethnicity.
Looking at that year’s new HIV diagnoses among gay and bisexual men more specifically by age, men between 30 and 39 accounted for 42 percent of the total cases, followed by the 20- and 29-year-olds at 25 percent of the cases and then men between 40 and 49 accounting for 21 percent. Men over 50 accounted for nine percent of the cases and men between 13 and 19 accounted for only three percent of the cases.
Participants in a series of Manhattan town meetings on gay men and HIV, starting in November of 2003, have regularly stated that most new HIV infections are happening among young, gay men, many of them African Americans. The city data appears to dispute that, but only partially.
Among gay and bisexual men who were 29 or younger, new 2002 diagnoses were concentrated to a significant extent among African-American men. Thirty-eight percent of the diagnoses in 20- to 29-year-olds were among African-American men, 33 percent were Latino, and 25 percent were white. In the 13- to 19-year-olds, 47 percent were African American, 44 percent were Latino, and nine percent were white.
The 2002 data shows a clear split at the age of 30 regarding the racial composition of new gay and bisexual HIV infections, a pattern also found in the 2001 data. Fully 80 percent of new diagnoses among gay and bisexual men under 30 in 2001 were among African-American and Latino men. White men accounted for only 17 percent of that total. However, for men over 30, white men accounted for 41 percent of the cases while African-American and Latino men accounted for 57 percent of the cases. The remaining percentages in both groups were unknown or other.
“The 2001 data show a race/ age distribution that is similar to the distribution observed in 2002 when, [among men who have sex with men under 30], incidence is primarily in minorities,” Dr. Lucia V. Torian, director of the HIV epidemiology program at the city health department, wrote in an e-mail. “[In MSM over 30], the race/ ethnicity distribution shifts to 41 percent white, 29 percent black, 28 percent Hispanic.”
There were 1,205 new HIV diagnoses reported among gay and bisexual men in New York City in 2002, the latest year for which such data is available. There were 4,684 new HIV diagnoses citywide and men who have sex with men accounted for 26 percent of the cases, followed by heterosexual transmission and then injection drug use.
But the data has limits, most notably the number of cases—2,203, nearly half—that are still under investigation and to which no risk factor has been assigned.
The data reflects the age of these men when they were diagnosed, not when they were infected. It is entirely possible that some men in their 20s are not getting tested until their 30s. The city has consistently seen that roughly 25 percent of New Yorkers who are newly diagnosed with HIV get an AIDS diagnosis within 31 days of their HIV diagnosis. These are people who clearly delayed getting their first HIV test for many years.
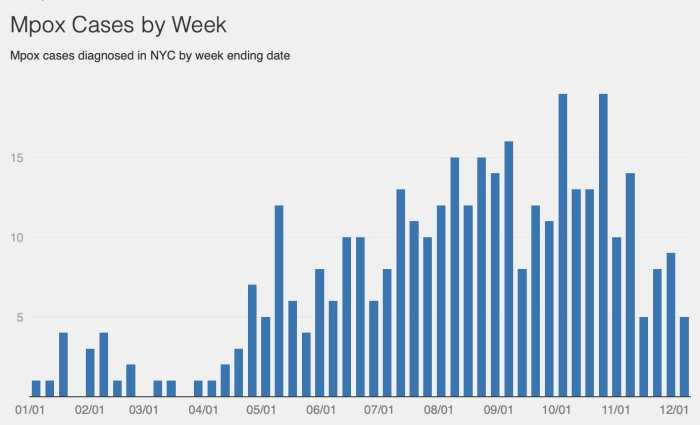
It has also been routine for people to warn that new HIV infections are rising among gay and bisexual men in New York City. Other city health department data does not support that.
Between 1993 and 2002, the incidence rate, or the percentage who are newly infected in a year, among gay and bisexual men has stayed at two to three percent.
“The good news is it’s not going up,” Torian said in an interview. “The bad news is it’s not going down.”
The incidence rate in both 2001 and 2002 was 2.4 percent. While that seems low, incidence is cumulative. After ten years at a 2.4 percent rate, 24 percent of the group being tested would be infected. For any community to have a quarter of its members chronically and seriously ill would be nothing less than a public health disaster. The incidence data reflect city health officials’ best estimates.
Gay City News shared the data on new diagnoses with AIDS researchers who found it intriguing while noting its limits.
“While there is some evidence that, among young MSMs, the new infections are somewhat more concentrated among men of color, the number of new infections in white men shows what I have long thought that the disease certainly continues to exist and spread in the white, gay male community,” wrote Dr. Perry N. Halkitis, a psychology professor at New York University and co-director at the Center for HIV/AIDS Educational Studies and Training (CHEST) in an e-mail.
Halkitis added that the data may be misleading.
For instance, the larger number of infections in 30- to 39-year-old men living in New York City could simply mean that there are more of those men living here.
Ultimately, however, the data says the community needs to broaden its focus when doing HIV prevention, according to Halkitis.
“We are short-sighted in simply saying HIV infections are now totally concentrated in young men of color,” Halkitis wrote. “Second, why are we shocked that older and white men are getting infected? They are also the ones who are relying heavily on club drugs and have embraced the barebacking culture.”
For Dr. Jeffrey T. Parsons, a co-director at CHEST and a psychology professor at Hunter College, the data on new HIV diagnoses could reflect a greater willingness on the part of 20- to 29-year-old African-American and Latino men to get tested while their white peers are delaying testing.
The data on the men over 30 might show that men in this age group have become complacent about or resigned to becoming infected.
“This is the population that experienced the first wave of HIV, and as such they’ve seen the dramatic changes in treatment, so perhaps they are less concerned about infection,” Parsons wrote in an e-mail. “It could also be that some of these men feel that they will eventually become HIV-positive anyway, so they worry less about protecting themselves.”