The progress made in the fight to end the HIV/AIDS epidemic by 2020 has slowed in recent years, according to one local healthcare leader who is calling for immediate action before it is too late.
Amida Care CEO Doug Wirth, who oversees the non-profit community health plan that covers more than 7,000 Medicaid recipients citywide, is pleased to see the rate of new HIV infections in New York City continue to fall every year. But the fine print shows him that there are some red flags.
“The rate at which new HIV infections drop is slowing down in New York City,” Wirth said in an interview with Gay City News.
“In 2016, we saw an 8.6 percent decline in infections, but in 2017 the drop slowed to 5.4 percent.”
In response, Wirth is calling for expanded eligibility for Medicaid Special Needs Plans (SNPs), which are tailored toward populations at higher risk to provide them with coordinated care to best fits their needs. Among the benefactors of SNPs include those with HIV/ AIDS as well as homeless people, and Wirth said the state should open SNPs to “anyone who is in need of enhanced care.”
Currently, the state’s blueprint on ending the HIV/ AIDS epidemic focuses attention on groups at high risk of infection, including men who have sex with men, transgender people, women of color, injection drug users, and couples where one partner is HIV-positive and the other one is HIV-negative. But HIV-negative trans people are the only HIV-negative ones among these groups who are eligible to enroll, according to Amida Care.
Two main parts of the effort to address HIV/ AIDS among vulnerable populations, according to Wirth, include making sure HIV-positive people are on medication and expanding access to PrEP, a daily pill that helps prevent the spread of HIV, among those who are negative.
“If you think about the South Bronx, if you think about Upper Manhattan, East New York, pockets in Queens and Staten Island, and the Lower East Side, those are all communities with higher viral loads,” Wirth said.
Wirth hopes the extra attention placed on the affected groups should prevent any spikes in HIV diagnoses.
“The idea is that if, in the same zip code that we have higher viral loads, we can support positive people becoming undetectable and enhance access to PrEP by LGBTQ folks, women of color, and trans people, that’s the way to end the epidemic,” he explained.
Wirth said that his team has thus far received a “great response” from the state Department of Health, its AIDS Institute, and state Medicaid director Donna Frescatore. But with 2020 on the horizon, time is running out.
“The real issue is that we have only got two years left,” Wirth said. “We would like to see the state advance this innovation as quickly as possible — by April 1 of this year. The question really is how quickly the state is able to innovate and complete the expansion. From our perspective, we can’t wait.”
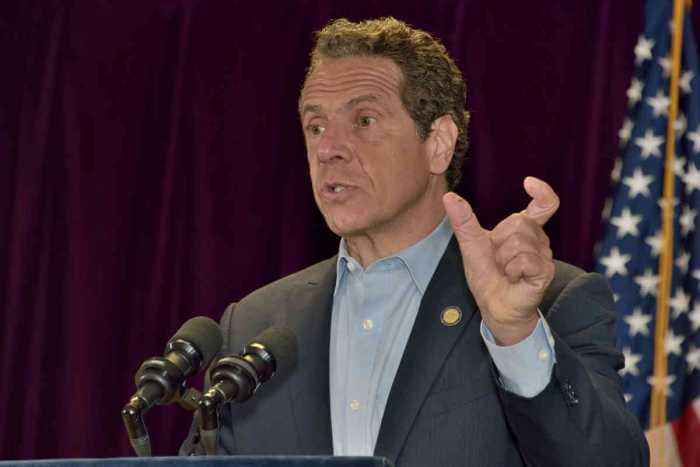
Governor Andrew Cuomo, who said in November that the state was still on track to end the epidemic by 2020, announced expanded access for HIV/ AIDS-related care. The state Department of Health increased the income threshold and eliminated the assets test to determine who is eligible for the HIV Uninsured Care Programs, which help HIV-positive people who are underinsured or uninsured.
But Amida Care believes access needs to be expanded further, and Wirth said the state has the authority to do so. When discussing the way communities of color are disproportionately affected by HIV/ AIDS, Wirth drew comparisons to the plight of white gay men in the 1990s when they did not have the tools necessary to prevent the epidemic from spreading.
“We can actually prevent HIV from spreading among young gay and bisexual men of color, among women of color, and we can take care of and support our transgender brothers and sisters to live their most authentic life,” Wirth said. “We have the tools, and Medicaid Special Needs Plans are best prepared to serve those communities.”
There are also other forces that could further complicate healthcare progress before 2020. The recent federal court ruling striking down Obamacare — currently stayed while the appeals process continues — has thrown a wrench into the future of the entire health care industry, for example, but Wirth stressed that Medicaid is “a strong program” and that people can expect their enrollment benefits to remain in place.
Wirth also emphasized that helping those who already have HIV can speed up the decline in HIV infections. Among those initiatives include focusing on expanding statewide housing initiatives for low income people with HIV and bolstering employment programs that can help HIV-positive folks get jobs.
“Employment programs can enable HIV-positive people with outreach, and to help walk people with an HIV diagnosis into care,” Wirth said. “People living with HIV have a rich array of life experiences.”
Stable housing has been shown be an especially critical factor in enhancing compliance with treatment regimens, allowing HIV-positive individuals to maintain an undetectable viral load and be non-infectious.