For yet another year, health providers serving New Yorkers are warning of chaos and dire consequences if the state moves ahead with a plan to overhaul a federal drug discount program for underserved clients in local communities.
The federal initiative, formally known as the 340B program, requires drugmakers participating in Medicaid to sell medication at reduced rates to managed care providers. In turn, those providers are directed to spend the savings on staffing and critical services for patients, such as transportation to and from appointments. Individuals living with HIV/AIDS, LGBTQ folks, and people of other marginalized backgrounds make up a significant share of individuals affected by 340B.
The program — which impacts community health non-profits, homeless shelter providers, and safety net hospitals — also facilitates a system in which the community health providers are able to collaborate with doctors and pharmacists to coordinate complex care for patients in need of tailored services. Patients with multiple health conditions, for example, can contact their providers when they are at the pharmacy to make sure they are getting the right prescriptions — and they can expect their issues to be resolved in a timely manner.
All of that, advocates say, would be in jeopardy if the state moves ahead with plans to implement a carve-out of the 340B program on April 1 of next year. Rather than funneling funds back to the community providers, the money would instead be given to the state as part of a fee-for-service model.
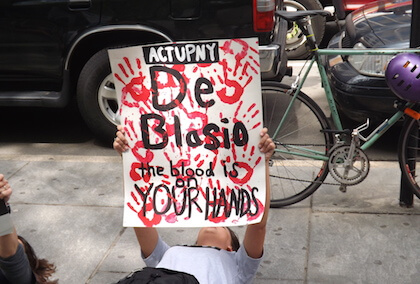
Advocates successfully managed to thwart the changes in recent years, but now they’re back to the drawing board — and they want the carve-out to be repealed entirely.

“If those dollars go away, then we are at risk for losing not just programs and services provided by safety net providers, but we are also at risk of losing safety net providers entirely because some of the HIV service providers will end up having to close their doors,” said Jacqui Kilmer, the CEO of Harlem United, which provides healthcare, housing, prevention, and supportive services to more than 10,000 clients every year.
Anthony Randolph, an Army veteran who lives in the Bronx, has seen the effects of the 340B program firsthand. He remembers a time when he was seriously ill and needed to pick up medication that was critical to his recovery, but the pharmacist said the prescription was already filled.
“I had to put my head up so tears wouldn’t come down,” Randolph explained during an interview with Gay City News. “There was nothing left in me. I was sick, my body was in pain, and I didn’t know what to do.”
However, Randolph said his health plan provider called his doctor and worked with the pharmacist to solve the issue — all thanks to the mechanisms in place for the 340B program.
Advocates say the potential consequences of the 340B changes are already evident in California, which just shifted control of its Medicaid prescription program at the beginning of the year. Magellan Health was tasked with handling 14 million patients and was immediately overloaded, leaving countless patients without their necessary medication and forcing them to wait on hold with a call center for up to eight hours, according to the Los Angeles Times.
New York-based groups are paying attention to the situation in California and warning the state’s leaders that such delays in care would have a major impact on their vulnerable clients.
“A lot of our clients are HIV-positive or on PrEP, so they can’t miss doses,” said Matt Bernardo, the president of Housing Works, which is a non-profit serving clients living with HIV/AIDS and experiencing homelessness.
Providers are plotting out their next move as they continue to make the case against the scheduled changes — and they are feeling pressed for time because although April 2023 is more than a year out, budgets are hashed out long before that date.
Kilmer said her team is planning to meet with State Health Commissioner Mary T. Bassett — who previously led the city’s health department — as well as representatives from the governor’s office.
Both Kilmer and Bernardo are hopeful that the governor will be open to repealing the Cuomo-era plan, but they conceded that its fate remains unclear.
“For some safety net providers, they will already have to implement cuts in services and staff just because this thing is looming out there and they’re not assured that they’re going to receive benefits,” Kilmer said.
Bernardo echoed those comments, saying it is difficult to plan when the future is so uncertain.
“This would be such a drastic change to the healthcare system in New York,” Bernardo said. “We are asking the governor to repeal it now.”
The governor’s office did not respond to requests for comment for this story.