The US Food and Drug Administration (FDA) has approved a bi-monthly injectable form of PrEP to prevent HIV infection, adding yet another tool in the fight against HIV/AIDS nine years after the agency first authorized daily PrEP pills.
The injectable PrEP regimen — intended to prevent HIV transmission through sex, not injection drug use — begins with one shot in back-to-back months before shifting to bi-monthly jabs. Patients also have the option of testing their body’s tolerance of the injectable drug, known as Apretude, by taking it orally for four weeks before moving to the shots.
The FDA’s approval of Apretude follows the emergence of studies showing strong efficacy for the shots in comparison to PrEP pills, which are already approximately 99 percent effective at preventing HIV through sex, according to the CDC. The injections will be available for at-risk adults and adolescents who weigh at least 77 pounds.
One study involving 4,566 cisgender men and transgender women who have sex with men concluded that Apretude was 69 percent better at preventing infection than Truvada, a daily HIV prevention pill. A separate study featuring 3,224 cisgender women who received Apretude injections found that their risk of HIV infection was 90 percent less than those who took Truvada. In both of the studies cited by the FDA, participants were given oral Apretude for up to five weeks.
The shots are getting approved less than a year after the FDA rubber-stamped a once-per-month treatment injection for individuals living with HIV.
According to the Centers for Disease Control and Prevention, 69 percent of new diagnoses in 2019 were among men who have sex with men, while straight individuals represented 23 percent of new diagnoses. Seven percent of new diagnoses were among those who inject drugs and trans folks made up about two percent.
Those between the ages of 25 and 35 represented the greatest share of new HIV diagnoses in 2019, with 13,127 — nearly twice as many as the 7,147 new diagnoses among people between the ages of 35 and 44. Twenty-six percent of new HIV diagnoses in the US were among Black individuals.
The bi-monthly shots could be easier to maintain than daily pills for PrEP. Some areas — including New York City and San Francisco — have outlined guidelines for a “PrEP on Demand” or “2-2-1” approach in which patients can take PrEP pills around sexual schedules instead of daily.
“This injection, given every two months, will be critical to addressing the HIV epidemic in the US, including helping high-risk individuals and certain groups where adherence to daily medication has been a major challenge or not a realistic option,” Dr. Debra Birnkrant, director of the Division of Antivirals in the FDA’s Center for Drug Evaluation and Research, said in a written statement.
The additional PrEP options could be useful in the government’s broader campaign to expand HIV prevention medication. Just 25 percent of those who are ideal candidates for PrEP have a prescription, which is still 22 percent improvement from 2015, according to the FDA.
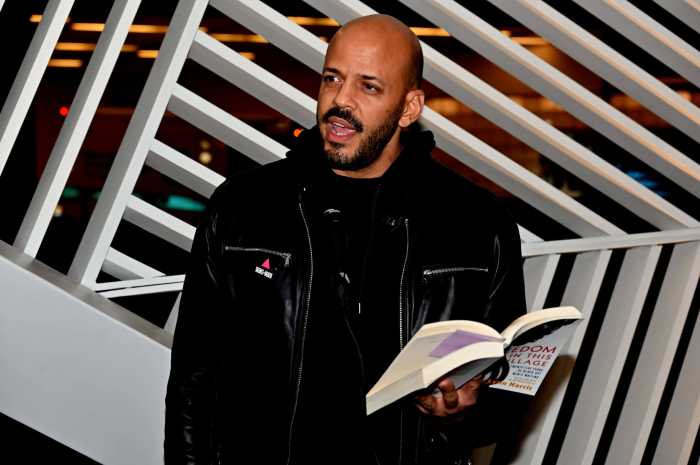
Nonetheless, advocates are speaking out about potential hurdles associated with injectable PrEP. It could be years before the general public has wide access to the shots, according to Kenyon Farrow, the managing director of advocacy and organization for PrEP4All, which advocates for PrEP access.
“We are definitely happy to see the FDA approval of another option for people who want to use PrEP,” Farrow said in a written statement. “The long-acting injectable taken as a shot six times a year may be a great choice for people who struggle with adherence to a daily pill or intermittent (2-1-1) pill use. But just as with the long-acting injectable for treatment that was approved one year ago, we anticipate the implementation of this option will likely take years to make it real for most people. Due to COVID, public health systems are already overburdened and much of the workforce needed to implement this large scale are leaving the field due to burnout.”
The injectable PrEP is being produced by Viiv Healthcare, which is owned by GlaxoSmithKline, Pfizer, and Shionogi. Viiv Healthcare plans to begin shipping Apretude to wholesalers and distributors within the United States early next year. It has not been approved outside of the country.
Those who plan to take Apretude will be required to undergo HIV testing prior to every shot. The drug contains labels warning consumers that individuals who have received the injections after becoming HIV-positive have been found to have drug-resistant HIV variants, so there is an emphasis on ensuring those who receive injections are indeed HIV-negative.
“Because it will need to be administered in clinical settings, it won’t be treated as a pharmacy benefit by payers, but instead as a medical benefit, which will take time to implement the proper coding for billing, as well as education and training for nurses who will likely bear the brunt of the work to implement,” Farrow added.
Those who take PrEP orally already have access to generic options and the Biden administration earlier this year directed insurers to provide PrEP at no extra cost, though not all Americans are covered. PrEP4All hopes the injectable PrEP will soon be covered without cost sharing.
In the meantime, Farrow said the injectable PrEP “will likely require prior authorization by most PrEP users, making it even harder to access for most people since the generic TDF/FTC is a fraction of that price.”
Study participants who received Apretude reported side effects such as back pain, fatigue, fever, headache, injection site reaction, myalgia, and rash, according to the CDC.
Further developments surrounding injectable PrEP could be forthcoming. Gilead announced last year that it was evaluating a drug called lenacapavir to be used as an injectable PrEP option administered once every six months, and Carl Schmid, a member of the Presidential Advisory Council on HIV/AIDS and the executive director of the HIV+Hepatitis Policy Institute, expressed optimism about that during an interview with Gay City News in November. There are also discussions underway, Schmid said, about a once-per-year implant to prevent HIV infection.