Suggesting that medical providers may be an obstacle to the wider use of pre-exposure prophylaxis (PrEP), panelists at a town hall noted that there is reluctance on the part of some doctors to prescribe the HIV prevention drug regimen and there is an ongoing challenge for patients to find providers who know what PrEP is.
“There are very few providers that have an expertise around this issue and there is a lot of provider ambivalence around anything having to do with sex,” said Carrie Davis, the chief programs and policy officer at the Lesbian, Gay, Bisexual & Transgender Community Center, at the November 19 event. “When people come forward and go to their provider, there’s a strong chance they’ll be met with rejection from the provider.”
Billed as a PrEP rally, much of the discussion touched on the struggles to get PrEP, which uses anti-HIV drugs in HIV-negative people to keep them uninfected, and the extent to which HIV stigma may be keeping people from accessing PrEP, which is highly effective when used correctly.
PrEP, along with post-exposure prophylaxis (PEP) and treatment as prevention (TasP), is a central component of the Plan to End AIDS, an effort that aims to reduce new HIV infections in New York State from the current roughly 3,000 a year to 750 annually by 2020. If doctors, who are the gatekeepers for PrEP prescriptions, resist writing prescriptions or are unaware of the intervention, that could have a significant impact on the plan’s success.
The panelists were unanimous in the view that finding a doctor who is educated about PrEP and will prescribe it can be difficult.
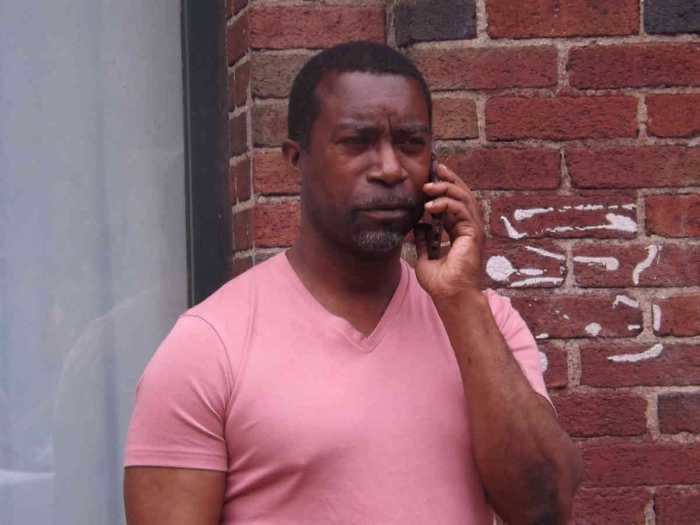
“A lot of my friends were having problems with their doctors prescribing it so I told them to find a gay doctor,” said Kashif Amin, who has been on PrEP for roughly a year, at the town hall.
Victor Hogue, a care technician at the Chelsea-Clinton health center operated by the William F. Ryan Community Health Centers, which sponsored the town hall, described his visit with a doctor after he began PrEP. Upon seeing that he was taking Truvada, the only drug approved for PrEP, she assumed he was HIV-positive. When Hogue explained that PrEP is an HIV prevention tool, the doctor said, “I don’t think that’s correct.”
New York City has seen recent increases in the number of gay and bisexual men who are using PrEP, but the growth has been modest, with much of the increase driven by uptake among white gay men. The state health department estimates that the number of New Yorkers who are enrolled in Medicaid, the government-run insurance plan for the poor, who are on PrEP has grown from 259 in 2012 to 1,330 in July of this year.
In an email, Gilead Sciences, which manufactures and markets Truvada, reports that “8,512 unique individuals started Truvada for PrEP in the United States between January 1, 2012, and March 31, 2015.” That estimate uses data from “39 percent of all US retail pharmacies that dispensed Truvada for PrEP.” Gilead’s estimates are seen as conservative by AIDS activists.
The company is reporting “a 332 percent increase in the number of unique individuals that started Truvada for PrEP in the United States between first quarter of 2014 to the first quarter of 2015.”
There is very little data on what doctors know about PrEP and their willingness to prescribe it. On a November 24 conference call with reporters, Dr. Anne Schuchat, the principal deputy director at the federal Centers for Disease Control and Prevention (CDC), discussed a 2015 survey of doctors and nurses by Porter Novelli, a public relations firm, that found that just 34 percent of the providers participating in the survey did not know about PrEP. The survey did not assess if the remaining two-thirds would prescribe the drug.
“Thirty-four percent were not aware of PrEP,” Schuchat said. “The idea that two-thirds are aware of it doesn’t mean that two-thirds are willing to prescribe it.”
The CDC convened the conference call to promote PrEP use, saying that too few people who would benefit from PrEP are on the drug.
“We need to work to ensure that clinicians are aware of PrEP,” Schuchat said. “Doctors need more prep about PrEP.”
PrEP requires that doctors ask patients about their sex lives and drug use and screen for any HIV risks. Then people on the drug must have quarterly visits with their doctors to check for side effects and to screen for sexually transmitted diseases.
“If you are not screening people for risk… and you’re not offering people who may be exposed to HIV PrEP, that kind of feels like malpractice to me,” Dr. Demetre Daskalakis, the assistant commissioner in the city’s health department who oversees HIV programs, said at the town hall. “This is not just an idea, it’s an expectation.”