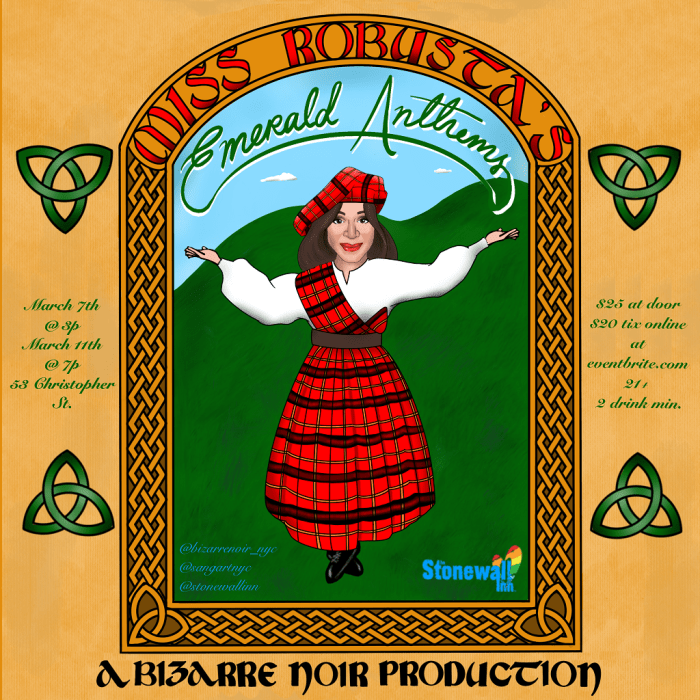
Dr. Demetre Daskalakis, the health department’s assistant commissioner for HIV/AIDS Prevention and Control, at the December 1 dedication of the NYC AIDS Memorial. | DONNA ACETO
BY NATHAN RILEY | If a phrase could capture New York City and State’s approach to bringing down levels of new HIV infection, it would be “drugs into bodies.” Pills in the form of pre-exposure prophylaxis are the closest thing to a vaccine that science has discovered. Instead of a single injection that last years, the same protection is offered with daily doses of antiretroviral medicines.
The number of new cases in New York City is declining; the 2,493 new infections identified in 2015 is a significant improvement, with that number previously stuck at about 3,000 each year. But the new number is only a start. A further decline of more than 70 percent will be needed if the city is to reach its goal of 600 new cases a year, in an effort where the statewide goal is 750. Reaching those goals, experts agree, would create an epidemiological state where the pool of new HIV infections would begin a consistent decline.
Such a dramatic drop will require sustained successful public health interventions. Small, steady steps must continue to build on themselves.
Health department emphasizes role of doctors, clinics in identifying at-risk patients
With numbers on the decline, however, it seems clear progress is underway, and the city’s Department of Health and Mental Hygiene has begun a demonstration project with the federal Centers for Disease Control and Prevention to leverage that progress. Officials don’t call it “drugs into bodies,” they use the buzzword “status neutral” – an intervention that involves expanding the avenues for getting pills to people who are HIV-negative.
One phase of that project reaches primary care physicians. According to Dr. Demetre Daskalakis, the health department’s assistant commissioner for HIV/AIDS Prevention and Control, drug reps have been hired to visit doctors to explain how two treatments work: PrEP or pre-exposure prophylaxis, offered to at-risk negative who person wants protection from infection, and PEP or post-exposure prophylaxis, a 28-day course of treatment for a person in the immediate aftermath of a potential HIV exposure.
The objective here is to get physicians more attuned to thinking about those patients they have who may be at risk for HIV. A patient who has an STD could be a candidate for PrEP; doctors shouldn’t wait for a patient to become infected. Hence the title: “status neutral.”
Patient screening for HIV risk should be on every doctor’s checklist, Daskalakis said, comparing that assessment to screening for diabetes. That disease can crop up at any age and is controlled by medication that doesn’t make it go away, but instead eliminates or mitigates its harmful effects. Primary care physicians are able to identify patients at risk for diabetes and treat them, without the patient having to see a specialist. The health department sees primary care physicians playing the same role in HIV prevention with PrEP, and its goal is to mobilize a greater number of health care professionals in screening for risk and taking preventive action.
Many of those most at risk, however, do not have primary care doctors, so the city is also dramatically improving services at its eight currently open STD clinics. At the start of 2016, funding and hours at the clinics increased, and in recent weeks a second phase began, with one clinic offering one-stop shopping for HIV testing and medication, an initiative of which the de Blasio administration can be proud. With the Chelsea clinic currently shuttered for major renovation, the Riverside clinic on West 100th Street, in particular, has been picking up the slack, and there the customary testing services have been supplemented with free medication as well as medical and social services.
According to Daskalakis, already three walk-ins have tested positive for HIV and were given a free month’s supply of antiretrovirals, with no co-pay, blood work was begun just as it would be in a doctor’s office, and a social worker was available to discuss the patients’ insurance coverage and options and to help locate a physician with whom they can continue their care.
PrEP and PEP are available at the Riverside clinic on the same basis. A patient who reports a recent HIV exposure – within no more than the previous 72 hours – is given the full 28-day PEP treatment regimen at no cost, and at risk patients interested in starting PrEP are given a month’s supply with no out-of-pocket expense.
When this approach is fully implemented across the city’s clinics, it will represent a big jump in efficacy of New York’s prevention and treatment outreach. In 2015, these clinics performed 45,956 HIV tests, with less than one percent coming back positive. Everybody asking for the test is a candidate for PrEP or PEP; under a “stay neutral” intervention, the message is that if you are in the game, medication should be considered. For the first time at any STD clinic, anyone getting tested can be offered medication on the spot.
Two more clinics will start the program in February, according to Daskalakis.
The number of HIV tests performed at all clinics during the first six month of 2016 was 21,296, a level unfortunately 2,385 less than the first half of last year – likely attributable to the temporary closing of the Chelsea clinic. Still, at the lower number, New York has the opportunity for significant outreach to at-risk residents. One very positive statistic is that among those patients who need to return for a second visit, 98 percent of them do so, a sign that the clinics are effective in establishing productive relationships.
The Riverside Clinic is at 160 West 100th Street between Amsterdam and Columbus Avenues and has long been open 8 a.m. to 3:30 p.m., Monday through Friday, and closed the first Wednesday of each month. As part of the city’s expanded clinic hours, it is now also open on Saturday, 8:30 a.m. to noon, and on Tuesday and Thursday evenings, from 5 p.m. to 7 p.m.