The Biden administration on Oct. 21 issued a new proposed rule that would require health insurance providers to cover an injectable form of the HIV prevention medication known as PrEP, marking a significant step forward in the ongoing campaign to boost uptake and end the epidemic.
The Biden administration’s proposed rule came as part of a broader announcement featuring other rule changes, including a requirement that many health insurance plans must cover over-the-counter contraceptives without a prescription.
As for PrEP, the proposal means private health insurers would have to cover the long-acting injectable form without cost-sharing, meaning there would not be out-of-pocket costs for patients. Like other proposed rules, the policy will now undergo a 60-day period during which the public can offer feedback.
For the last decade, PrEP has been available in oral form — and while it has been a key tool in the fight against HIV, it has had an uneven rollout: By 2019, just 8% of Black people and 14% of Latinx individuals who were candidates for PrEP received prescriptions for it, compared to 63% of white people, according to federal research. Adhering to a daily pill has also proven to be a key challenge, prompting some health departments to float a PrEP-on-demand approach in which people can take the oral medication around the time when they have sex.
However, injectable PrEP removes the daily requirement — and research has indicated that the injectable version is extremely effective. There are different injectable PrEP medications: Gilead’s injectable drug, Lenacapavir, is administered twice a year, and ViiV Healthcare’s Apretude, or cabotegravir, is administered once every other month instead of twice annually. The twice-per-year shot still awaits Food and Drug Administration (FDA) approval.
The Biden administration’s proposed rule represents the latest attempt to improve access to PrEP. The Biden administration issued guidance in 2021 directing health insurers to cover PrEP at a time when the oral form was the only option widely available to consumers. In 2019, then-New York Governor Andrew Cuomo eliminated out-of-pocket PrEP costs for individuals with health insurers governed by New York State regulation.
Last year, an independent panel of experts known as The U.S. Preventive Services Task Force (USPSTF) gave injectable PrEP an “A” rating, which helped pave the way for the proposed rule because the Affordable Care Act requires insurers to cover drugs with an “A” or “B” rating.
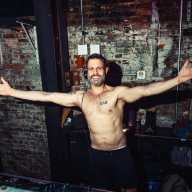
Callen-Lorde Community Health Center, which provides sensitive, quality health care and related services for LGBTQ New Yorkers regardless of ability to pay, hailed the proposed rule. Patrick McGovern, Callen-Lorde’s CEO, said in an interview with Gay City News that the proposed rule would help prevent health insurance companies from insisting on a specific kind of PrEP medication when initiating PrEP services.
“This rule is incredibly consequential, and we’re really happy to see it from the federal government,” said McGovern, who noted that Callen-Lorde is responsible for 15% of New York State’s PrEP prescriptions.
McGovern expects patients to flock to the injectable option once the rule is finalized and the new insurance requirements go into effect — and later on the twice-a-year injectable option could draw even more people.

“Even now, with the duration of two months of protection with an intramuscular injection, the demand has been much higher than we anticipated,” McGovern said. “The demand is just going to increase exponentially.”
Whether the injectable version of PrEP will be successful remains to be seen, but it could help two current issues with PrEP, McGovern explained: Many of the people who are at risk of contracting HIV are not even trying PrEP, while others are finding it difficult to keep up with the oral pills and the lab work necessary to maintain a prescription.
Individuals experiencing homelessness, mental health conditions, and other issues can find it difficult to adhere to the daily pill regimen. The injectable option can reduce those visits to as few as two times per year if the twice-annual shot is covered, McGovern said.
“Today you can have protection with just an injection once every two months,” McGovern said. “It’s a huge breakthrough, but nothing like what’s coming where you know it could be a twice-yearly injection… These are going to be truly, truly transformative.”
McGovern said Callen-Lorde plans to ramp up a marketing campaign to spread awareness about injectable PrEP, including when the longer-term injectable becomes a reality. The awareness effort’s target audience will include young, Black and Latino gay men, as well as transgender individuals.
“There’s more time to be able to deal with those coverage barriers, so for people who are of highest need, persistent coverage is a challenge,” McGovern said. “So I think we’ll be able to more aptly reach the populations that are most at need.”