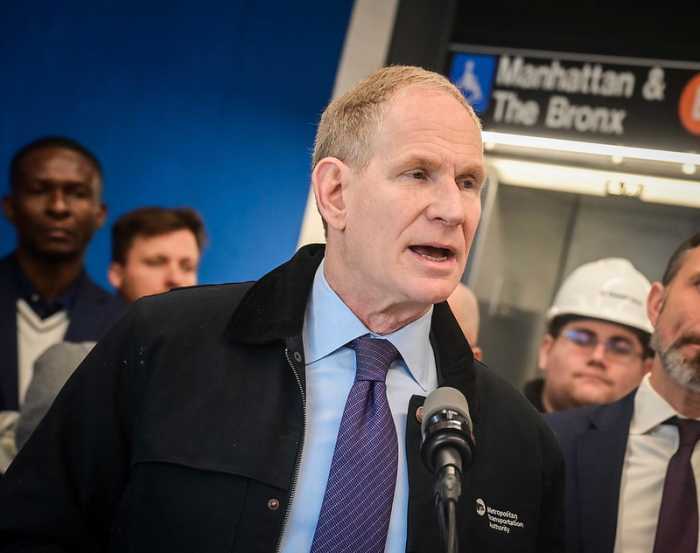
Governor Andrew Cuomo at last June's Pride Parade announcing New York’s commitment to a plan to effectively end the AIDS epidemic by 2020. | GAY CITY NEWS
BY DUNCAN OSBORNE | The proposed New York state budget for the fiscal year that begins on April 1 includes $5 million for a pre-exposure prophylaxis (PrEP) program serving populations at high risk for HIV infection, but documents suggest the state will cap the number of annual participants in the program at 600, a number that by itself is too low to have a significant impact on HIV infections in the state.
“Prevention is the most important element,” said Guillermo Chacon, president of the Latino Commission on AIDS, referring to a state plan to reduce the number of new yearly HIV infections from the current 3,000 to 750 by 2020. “We want more than that.”
The proposed PrEP Assistance Program, which was discussed in Governor Andrew Cuomo’s Opportunity Agenda, a budget document, “will help 600 persons per year stay negative, and with Medicaid and other insurance products, complete a system that will help ensure as many highest risk persons as possible have good access options.”
Drug Assistance Program may assist as few as 600 on preventive meds
Medicaid, the government health plan for the poor, will contribute $2.5 million to the program and the AIDS Institute, which is part of the state health department, will contribute $2.5 million, according to the state budget office. One anti-HIV drug, Truvada, is approved for PrEP. Taken daily, Truvada is highly effective at keeping HIV-negative people uninfected.
The AIDS Institute did not respond to an email asking, among several questions about the program, if the 600 is a cap and what the other elements of the “system” will be, though the state will clearly rely on private insurance and Gilead Sciences, Truvada’s manufacturer, to pay for PrEP for many users.
“Currently, Medicaid and other high quality insurance products cover PrEP, and the drug manufacturer offers both assistance obtaining the medication and covering co-pays, but there remain specific barriers to wide adoption of this highly effective prevention,” the budget document said. “The PrEP Assistance Program will fill the gap among the various options by helping persons with lower grade insurance products cover the cost of services that have out of pocket costs associated with them such as HIV, STD, and kidney function tests.”
People taking PrEP get quarterly tests for sexually transmitted diseases and to see if Truvada has impacted their kidney functioning. The drug is also expensive, with estimated costs running as high as $12,000 a year.
Last year, Cuomo endorsed the plan to cut infections, which was sought by leading AIDS groups. Like Cuomo, AIDS groups want more dollars for PrEP, post-exposure prophylaxis (PEP), which uses anti-HIV drugs in a person with a recent exposure to HIV to prevent infection, and treatment as prevention (TasP). Under TasP, people with HIV who adhere to anti-HIV drug dosing schedules are effectively not infectious. Cuomo has emphasized the role of the three drug regimens in getting to 750, while AIDS groups have also sought, with limited success, more supportive housing and expanded access to government benefits for people with HIV.
In 2012, the latest year for which the state has data, 95 percent of the 3,316 new HIV diagnoses in New York were in New York City and 55 percent of the city diagnoses were among gay and bisexual men. To get to 750, thousands of gay and bisexual men will have to be on PrEP and the number of HIV-positive people who are taking anti-HIV drugs and have no detectable HIV in their blood will have to increase substantially. The rate of new HIV diagnoses among gay and bisexual men in the city has remained stubbornly high for 13 years while ever other transmission risk category has seen declines.
In 2014, the city health department surveyed 500 gay and bisexual men aged 18 to 40 and found that up to 59 percent were unaware of PrEP. Less than five percent reported using PrEP or PEP in the six months prior to taking the survey. The city health department launched a campaign to educate doctors about PrEP and PEP in early January.
Data from Gilead and the state health department suggest that PrEP use has increased in New York and across the country since the drug regimen was approved in 2012, though no one is suggesting that New York is close to the level of PrEP uptake needed to see large reductions in new HIV diagnoses.
A similar program in Washington State provides a useful contrast to the New York program. Washington, which hopes to reduce new HIV diagnoses by half by 2020, is spending $2 million annually on a PrEP assistance program originally aimed at helping 200 gay and bisexual men. That program began last year. As Washington found that more applicants were insured and only needed help with co-pays or quarterly tests, the program may be able to cover 300 people annually for the same budget.
“We will likely end up covering a lot more with the $2 million,” said David Kern, manager of the Infectious Disease Prevention Program at Washington’s state health department.
In 2013, Washington reported 470 new HIV diagnoses, with 395 among men and 273 of those among gay and bisexual men.