Roughly half of the people living with HIV in the United States were not virally suppressed and more than a third were not receiving treatment for the infection, according to new CDC data released this month stemming from 2015 and 2016.
The model-based data, which highlights the gaps in HIV care nationwide, further noted that 14.5 percent of the 1.1 million people with HIV were undiagnosed. Folks without a suppressed viral load made up 49 percent of HIV-positive individuals, and 37 percent of all HIV-positive folks were not receiving care.
The CDC’s estimated population breakdown of the HIV data indicated that 645,000 of the 1.1 million people with HIV in America during the timeframe of the study were men who had sex with men. The next largest group was straight women, who made up 194,200 of the total people infected. Straight men trailed behind at 87,500.
When divided up by age, there was a clear pattern: HIV infections were most prevalent among adults above the age of 55, but decreased with every age demographic from that point on down. Those above the age of 55 constituted 405,500 of the people with HIV compared to 258,000 of people between 45 and 54. Meanwhile, 65,200 people between the ages of 13-24 were infected — but that group also experienced the highest transmission rate.
Despite the range of data about various demographics, the CDC notably did not provide any race or ethnicity-based statistics. In a separate report about PrEP, an HIV prevention medication taken daily, the CDC noted that black and Latino gay and bisexual men at high risk of acquiring HIV were 10 to 14 percent less likely to take the pill than high-risk white men. Black and Latino men also were less aware of PrEP than white men.
The study provides no guidance on how much the numbers may have changed since the 2015-2016 data was obtained. The CDC’s most recent releases pertaining to HIV/ AIDS are focused on data that is between two and four years old.
HIV-based health care organizations and providers, including Gay Men’s Health Crisis, Callen-Lorde Community Health Center, and Harlem United did not respond to requests for comment on the CDC data.
The lack of treatment among such a large swath of HIV-positive people in America could reinforce many of the concerns raised by experts in the field.
Financial impediments have often been cited as major hurdles to HIV treatment. The price of PrEP has climbed significantly in recent years, prompting calls for a generic version of it in order to boost accessibility. And some of the people who are living with HIV have a difficult time affording their medication.
The latest statistics from the CDC coincide with President Donald Trump’s recent announcement of a plan to end the HIV/ AIDS epidemic by 2030. The plan has been met with wide skepticism among HIV/AIDS advocates, and Amida Care, a non-profit community health plan serving roughly 7,000 HIV-positive Medicaid recipients in New York City, blasted the administration even further on March 18. The organization noted that Trump’s proposed cuts in the areas of housing, Medicaid, and Medicare significantly undercut the effort to curtail the epidemic.
“Actions speak louder than words: to end the epidemic, the administration must align its actions with its rhetoric,” the organization wrote in an email outlining major concerns about the president’s cuts. “To end the epidemic, the president must stop attempts to undermine access to health care.”
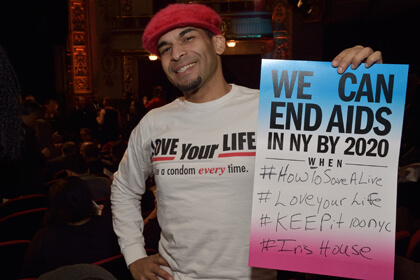
Locally, the State of New York claims to remain on pace to end the epidemic by 2020, with data released in October 2018 indicating the number of people diagnosed with HIV dropped 39 percent from 2007 to 2017. However, Amida Care, among other experts, has noted that the rate at which new infections have dropped is slowing down.
One striking cautionary note in New York State’s numbers is that 20 percent of people diagnosed with HIV statewide were also diagnosed simultaneously with AIDS, meaning that one fifth, as an absolute minimum, of people living with HIV are unaware of their status. That number is more than five percentage points higher than the nationwide rate of people who were undiagnosed.