While the de Blasio administration is celebrating a record low number of new HIV diagnoses in New York City in 2018, the city is faced with the daunting task of producing a substantial reduction in new HIV infections over the next two years to get to its goal of 600 new HIV infections a year by 2020.
“New HIV diagnoses are DOWN to record lows in New York City!” the mayor’s press office wrote in a November 22 tweet. “This is fantastic news, but there’s more work to be done.”
The city health department’s annual HIV surveillance report for 2018 disclosed that there were 1,917 new HIV diagnoses in New York City in 2018. That is an 11 percent decrease in reported new HIV diagnoses over 2017 and the first time that such diagnoses fell below 2,000.
Mayor Bill de Blasio and Governor Andrew Cuomo endorsed the Plan to End AIDS in 2014. That ambitious proposal seeks to reduce the number of new HIV infections to 750 a year statewide in 2020. With most new HIV infections occurring in the city, the city health department proposed to reduce new HIV infections to 600 in the city in 2020. While the plan’s progress is measured with a number of metrics — and a good number of those are showing success — ending the epidemic requires a large reduction in new HIV infections.
New diagnoses result from infections that occurred in the year they are reported and those from any earlier year not previously diagnosed. New infections that occur in a year are always estimated.
The 2018 report estimated that there were 1,600 new HIV infections in the city last year. Getting to 600 new HIV infections in 2020 would require the city to reduce new HIV infections by 63 percent in just two years. Going back to 2015, the city has seen year-over-year reductions in new HIV infections ranging from a high of 17 percent to a low of 12 percent, indicating that a reduction of more than half in a two-year period is unlikely.
In October, the Cuomo administration released data that touted a decline in new HIV diagnoses in 2018. A story in The New York Times read, “State health officials say they believe they are on track to lower the number of new HIV diagnoses to a little more than 1,500 per year by 2020,” which suggested that the state had changed its goal. In an October interview, however, Johanne Morne, the director of the state AIDS Institute, a unit of the state health department, told Gay City News that getting to 750 new HIV infections in 2020 remains a goal.
The city report illustrates a continuing struggle — reducing new HIV infections among African-American and Latino men who have sex with men. Among the 1,917 new HIV diagnoses in 2018, 1,484, or 77 percent, were among men. Among men, 1,191, or 80 percent, of the new HIV diagnoses were among African-American and Latino men. Sixty-seven percent of the new diagnoses in men, or 997, were attributable to men who have sex with men. Another 375, or 25 percent, had an unknown transmission risk.
The city has been successful in reducing new HIV infections in every other risk category or demographic, including among white gay men, to the point that the city will not get to 600 new HIV infections in 2020 if it does not significantly reduce infections among African-American and Latino gay and bisexual men.
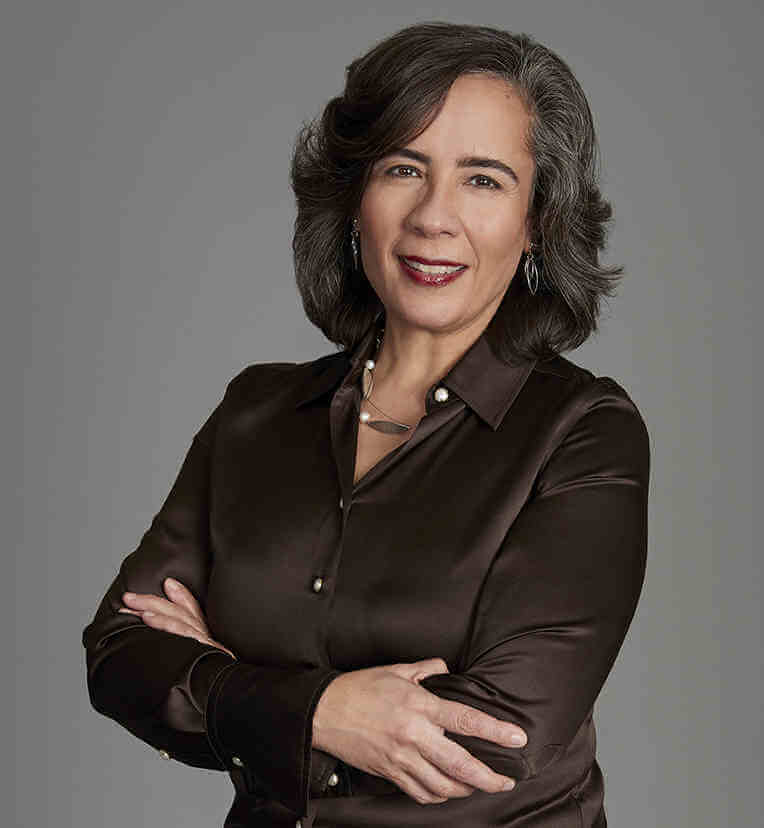
In the press statement that accompanied the report, Dr. Oxiris Barbot, the city’s health commissioner, recognized that.
“We take a data-driven, sex-positive approach to HIV prevention that is firmly grounded in equity and we are proving that it works,” Barbot said in that November 22 statement. “New York City can end the epidemic if we continue to fight against the stigma, bias, and discrimination that continue to be significant drivers of HIV, particularly among Black and Latino men who have sex with men.”
The Plan to End AIDS calls for treatment for people who are HIV-positive so they remain healthy and cannot infect others. The plan also supplies nutrition, housing, and other services that make staying on HIV medications easier. For prevention among people who are HIV-negative, the plan offers pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP), among other services. PrEP and PEP are anti-HIV drugs used to keep people uninfected. Both drug regimens are highly effective when used correctly.
While the data on PrEP use is limited, it suggests that obstacles remain among African-American and Latinx men and women to PrEP uptake. Some advocates fault the efforts to deliver PrEP to communities of color.
“To an extent not seen before, HIV has become a disease of poverty disproportionately affecting communities of color,” Ritchie Torres, an out gay member of the City Council who represents part of the Bronx, told Gay City News. “The Bronx alone is home to 24 percent of New Yorkers living with HIV. The focus of public policy should be on breaking down the barriers to accessing PrEP that continue to plague communities of color.”